Dogmas and Controversies in Hematologic Malignancies: Addressing Major Debates in Leukemia, Lymphoma, and Myeloma
Author
Binaytara Team
Introduction
This interview with Dr. Danilov focuses on controversial topics in lymphoma, leukemia, and myeloma, emphasizing the need for debates to address these controversies. Dr. Danilov highlights the importance of training and education for administering new therapies safely and the need for diverse patient representation in clinical trials. On March 28th, he will co-chair a CME-accredited conference in Los Angeles titled ‘Dogmas and Controversies in Hematologic Malignancies.’ Some of the key debates that will be covered include the use of bispecific antibodies versus CAR T-cells in follicular lymphoma and the integration of novel agents like BTK inhibitors in mantle cell lymphoma.
Highlights of Interview
Conference Focus and Controversial Topics
The "Dogmas and Controversies in Hematologic Malignancies" conference gathers West Coast and Mountain Region experts to discuss unresolved issues in lymphoma, leukemia, and myeloma. The conference fosters case-based discussions and interaction with both practitioners and industry professionals to address key controversies, such as the sequencing of CAR T-cell therapy and bispecific antibodies for lymphoma treatment.
Advancements in Hematologic Treatments and Implementation
With the rise of sophisticated therapies, proper education, and training are essential for safely administering new treatments. While immuno-oncology and targeted therapies have revolutionized cancer treatment, there Is a need to expand these therapies to broader patient populations. Additionally, cancer has become a manageable chronic condition for many, with treatments improving survival rates and offering hope for a cure.
Hematology and Patient Messaging
The appeal of hematology lies in its ability to visually diagnose diseases through blood smears and bone marrow biopsies, combining scientific curiosity with patient care. For patients, especially in the early stages of a diagnosis, the most important message is one of hope—cancer is treatable, and in some cases curable, with many patients returning to a normal life after treatment.
Interview
Question | Binaytara: What is the purpose and structure of the Dogmas and Controversies in Hematologic Malignancies conference?
Answer | Dr. Danilov: “The conference brings together West Coast and Mountain Region experts to discuss unresolved issues in lymphoma, leukemia, and myeloma. It fosters case-based discussions, practitioner and industry engagement, and aims to address key controversies in these diseases. As co-chair, I oversee the agenda for lymphoid malignancies, while my colleagues at City of Hope and UCSF lead sessions on leukemia and myeloma. Our expert panel collaborates to challenge existing dogmas, debate controversies, and explore solutions that can impact real-world clinical practice.”
Q: Could you share an example of a hotly debated topic in hematologic malignancies today? Also, since the agenda includes several debates, could you discuss why you chose that format and how it ties into the theme of controversy?
A: “There are several ongoing debates in hematologic malignancies. In diffuse large B-cell lymphoma and follicular lymphoma, the emergence of bispecific antibodies and CAR T-cell therapy has reshaped treatment strategies. CAR T-cells have largely replaced autologous stem cell transplants for many patients, but bispecific antibodies offer advantages such as off-the-shelf availability and easier administration. A key controversy is determining the optimal sequencing of these therapies—should bispecific antibodies be used before or after CAR T-cells? While CAR T-cells are limited to specialized centers, bispecific antibodies could potentially be administered widely, making them more accessible.”
Q: One of our goals at Binaytara is to advocate for the advancement of implementation science. Given your work in translating 'bench to bedside' research, what key changes do you think are needed to improve the translation of scientific and clinical research?
A: “That’s a very broad question. As treatment modalities become more sophisticated, with distinct side effect profiles and administration schedules, proper training and education are crucial. Establishing systems at individual sites to safely administer these therapies is essential.
In the past, cancer treatment was largely limited to chemotherapy and immunotherapy, with specialized centers handling transplants. Physicians became accustomed to managing predictable side effects like neutropenia. However, the emergence of immuno-oncology brought a dramatic shift, particularly in solid tumors and hematologic malignancies. Now, with the rise of cell therapies, bispecific antibodies, and targeted treatments, another wave of education is necessary to ensure these advancements reach patients in the community.
In academia, it’s easy to assume every resource is readily available, but real-world accessibility is a challenge. Clinical trials often skew toward specific populations and institutions, limiting broad representation. To improve equity, we must design trials that engage diverse patient populations and extend participation to community settings. This approach not only enhances trial diversity but also equips community physicians with hands-on experience in administering new therapies.”
Q: Are there any misconceptions people have about blood cancer that you would like to debunk?
A: “Interesting! I think one of the common misconceptions that people still hold is that having blood cancer is a death sentence. While acute leukemia is a difficult disease, it is no longer the case with the cutting-edge therapies we have, such as immunotherapy and chemotherapy. Many of these treatment approaches are actually curative in lymphoid malignancies or can induce long-term remission.
Although cancer remains a serious disease, advancements over the past 20 years have transformed it into a manageable chronic condition, similar to diabetes or hypertension. While some cancer subtypes still require improved treatments, efforts now focus on enhancing efficacy, achieving cures, and developing less toxic yet equally or more effective therapies. Many patients remain on treatment for life, challenging the misconception that cancer is always a death sentence. In reality, survival rates have significantly improved, and life expectancy for many patients has increased.”
Q: We would like to learn why you chose hematology and why you decided to become a doctor. I think it is important, especially considering the common misconception that cancer is a death sentence. There is also the idea that working in this field means losing more patients than in other specialties.
A: “The ability to help patients live longer, manage their symptoms, and sometimes achieve remission—things that weren’t possible 25 or 30 years ago—brings a lot of satisfaction. On top of that, oncology allows me to blend scientific curiosity with real-world applications: understanding how the body works, how disease operates, and how treatments can work and resist resistance. There is no other field like it.
Even when things don’t work out, there’s an opportunity to make decisions that ease suffering, make life better, or help patients through the end of life. I find that deeply meaningful. As for hematology specifically, I’ve always been fascinated by how diseases can be seen so clearly in blood smears and bone marrow biopsies. The visual aspect of it has always captivated me.”
Q: What message resonates most with patients during the early stages of their diagnosis, especially when they are overwhelmed or anxious about having cancer?
A: “The most important message is one of hope. It may sound ironic coming from a cancer center named City of Hope, but it’s truly relevant. With current treatments, hope is very real. Although a cancer diagnosis is never easy and is always disruptive, it’s important to convey that cancer can be treated, and in some cases, even cured. The hope of returning to a normal life is a powerful motivator for many patients as they begin their journey.”
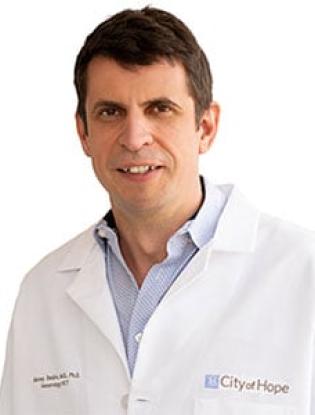
Alexey Danilov, M.D., Ph.D.
About Dr. Danilov
Dr. Danilov is a board-certified clinician and accomplished researcher specializing in chronic lymphocytic leukemia, mantle cell lymphoma, and non-Hodgkin lymphoma. As a Leukemia & Lymphoma Society Scholar, he serves as the Principal Investigator on multiple grants from the National Cancer Institute, Leukemia & Lymphoma Society, American Society of Hematology, and Lymphoma Research Foundation. He has spearheaded numerous clinical trials focused on novel targeted therapies and immunotherapies. Collaborating with the National Cancer Institute and the pharmaceutical industry, along with his leadership role in the Lymphoma Committee at Southwest Oncology Group, Dr. Danilov actively contributes to global drug discovery efforts. His laboratory emphasizes "bench to bedside" research, where preclinical discoveries pave the way for early-phase clinical trials, ultimately transforming scientific advancements into tangible treatments for patients.