Federal Healthcare Policies, Advocacy Efforts, and Cancer Care Affordability Highlighted at SCHD25 Finale

Author
Binaytara Team
Cancer diagnosis is disruptive. Healthcare is increasingly focused on profitability. Education for elected officials is insufficient. These were the themes that collectively wove through all sessions on Day 3 of the Summit on Cancer Health Disparities (SCHD25).
Lively Poster Presentations Showcase Innovations in Cancer Health Equity
As the day began, the conference hallways were filled with lively discussions from poster presenters sharing their work on minimizing cancer health disparities, from barriers to breast and cervical cancer screening to overcoming disparities in access to CAR T-cell therapy in diverse populations. Institutions across the U.S. were represented at the poster sessions, with presenters spanning every stage of the medical career path: medical students, residents, fellows, attendings, and faculty.
Poster presentations at SCHD25
Session 13: Policy as a Tool for Advancing Cancer Health Equity
The first session of the day was filled with meaningful discussions and powerful questions that left the room heavy with reflection. Chaired by Dr. Willie Underwood III, a board-certified urologist and health policy expert, Session 13 focused on the role of policy in supporting cancer health equity. Dr. Underwood’s keynote address explored the multifaceted nature of health disparities and the impact of health policy on patient outcomes.
The panel discussion that followed expanded on these themes, dissecting systemic issues in healthcare. Featuring a medical malpractice attorney, Archie L. Rich II, and a Standford breast cancer physician and professor Dr. Mark Pegram, the panel emphasized the critical balance between personal responsibility and social justice. Calls to action echoed from the stage, urging for strong partnerships to drive beneficial policy changes and for the development of strategic plans to manage rising healthcare costs.
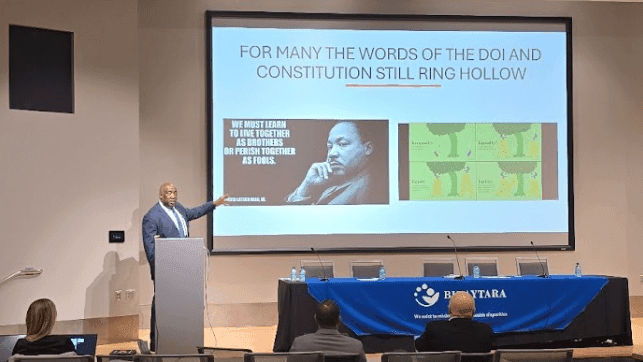
Dr. Underwood sharing the importance of social justice in healthcare
Session 14: Building Effective Advocacy Campaigns for Lasting Change
In a seamless progression of topics, Session 14 turned to the "how" behind the "what." Chaired by Dr. Dan Milner, Executive Director of the ATOM Coalition, the session focused on "Developing Effective Advocacy Campaigns." Lisa Lacasse, keynote speaker and president of the American Cancer Society Cancer Action Network (ACS CAN), emphasized the importance of connecting with elected officials through a combination of personal stories and data. She shared examples of both successful and unsuccessful advocacy efforts, including the ongoing push to expand Medicaid coverage in lower socio-economic states.
The panel also featured Tricia Johnson, executive director of Northwest Hope and Healing, and Jourdan Cruz, program therapist at the Healing Center, to highlight diverse perspectives on advocacy. Tricia discussed the staggering costs associated with cancer diagnosis and treatment and her organization's work to alleviate patients' financial burdens. Similarly, Jourdan talked about the launch of a suicide prevention program at the University of Washington, which focuses on universal mental health screening for all patients.
After several intellectually stimulating exchanges between the panelists and the audience, the session concluded with a call to action: to use personal experiences and collective voices to influence public policy and reduce the cancer burden.
SCHD25 Closes with a Powerful Debate on the Future of Healthcare
As a fitting close to SCHD, the most anticipated session— Debate - Crisis in Care: Can the U.S. Find a Sustainable Model for Affordable Healthcare?— began with a cordial, firm, and robust discussion about the U.S healthcare system. Moderated by CBS 48 Hours correspondent, Anne-Marie Green, and featuring renowned experts Dr. Alan Balch, the Chief Executive Officer of the Patient Advocate Foundation, Dr. Anders Kolb, the president of the Leukemia & Lymphoma Society, and Dr. Larry Kessler, professor of Health Systems and Population Health at University of Washington, the debate took on some of the pressing issues that persist and widen cancer care disparities. Key points included the need for a robust conversation on sustainable models for affordable care, the importance of social innovation, and the challenges of accessing innovative cancer treatments. The discussion highlighted the inefficiencies in the current healthcare system, the need for a unified national policy, and the potential benefits of a single-payer system. The panel also discussed the role of community health workers and the importance of addressing affordability gaps, particularly in vulnerable communities.

The debate moderator and panelists
In the lightning round, the expert panelists offered brief and impactful statements on several questions, such as which countries the U.S. should consider when looking to improve its healthcare system. The speakers pointed to the Netherlands, Australia, and South Korea — countries known for their strong systems that balance access, quality, and cost. The question then shifted to whether a single-payer or multipayer system is more scalable. The consensus? Competition alone does not resolve healthcare issues. A single-payer system could work, but it would need to be robust, efficient, and carefully designed to succeed on a large scale. When it came to the question of whether healthcare is a human right or a commodity, the speakers made it clear: it is not an either-or situation. Ultimately, the focus must be on healthcare as a right, ensuring access and dignity for all.
There was also a thoughtful rebuttal regarding prevention, particularly in blood cancers. The speakers emphasized that while prevention is important, much of the progress in blood cancers has come from innovation and access to new treatments, not just from prevention efforts.
Audience questions brought even more energy into the room. One question centered on the unionization of healthcare workers to protect professional interests. Another asked: Who really holds the power to improve healthcare? Dr. Kolb pointed to the FDA, and Dr. Kessler remarked in agreement. Overall, the takeaway is that the power lies in the hands of voters, whose choices will ultimately shape both federal and state healthcare policies.
As the session wrapped up, the speakers were posed a final, imaginative question: if you had endless money, how would you redesign the healthcare system? Dr. Kessler said he would launch a massive education campaign. Dr. Kolb emphasized that while health literacy is important, how patients access care matters even more. Dr. Balch highlighted the need to integrate social care into healthcare, investing in communities, patient navigators, and other supports that address the whole person.
The session ended with a feeling of gratitude for everyone who showed up, engaged in the conversation, and thought critically about the future of healthcare. The speakers left the audience with a challenge: building a healthcare safety net is an opportunity, not just a duty. Everyone should be thinking about how to close the affordability gaps in healthcare.
Finally, the winners of the poster presentations were announced, wrapping up the session on a celebratory note.
Disclaimer: The views and opinions expressed by the panelists are their own and do not necessarily reflect the official positions of their affiliated institutions. Some responses are based on the panelists' expertise and professional experience.