The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
Best of ASCO Seattle 2025: Key Hematologic Cancer Updates on Myelodysplastic Syndromes and Leukemia

Overview
Binaytara held one of its Best of ASCO continuing medical education events in Seattle, Washington—a powerhouse for medical oncology innovations. This conference was chaired by Dr. Petros Grivas and Dr. David Zhen from Fred Hutchinson Cancer Center and the University of Washington.

Dr. Petro Girvas

Dr. David Zhen
With the recent conclusion of the ASCO annual meeting, Best of ASCO Seattle aimed to explore new and updated treatment options for patients with hematologic malignancies and solid tumors. The meeting also reviewed abstracts presented at ASCO 2025, focusing on how these findings can be applied in clinical settings.
Below are highlights from the Session 1 presentation on MDS and Leukemias by Dr. Roland Walter, a professor in the translational science and therapeutics division at Fred Hutch Cancer Center.

Dr. Roland Walter
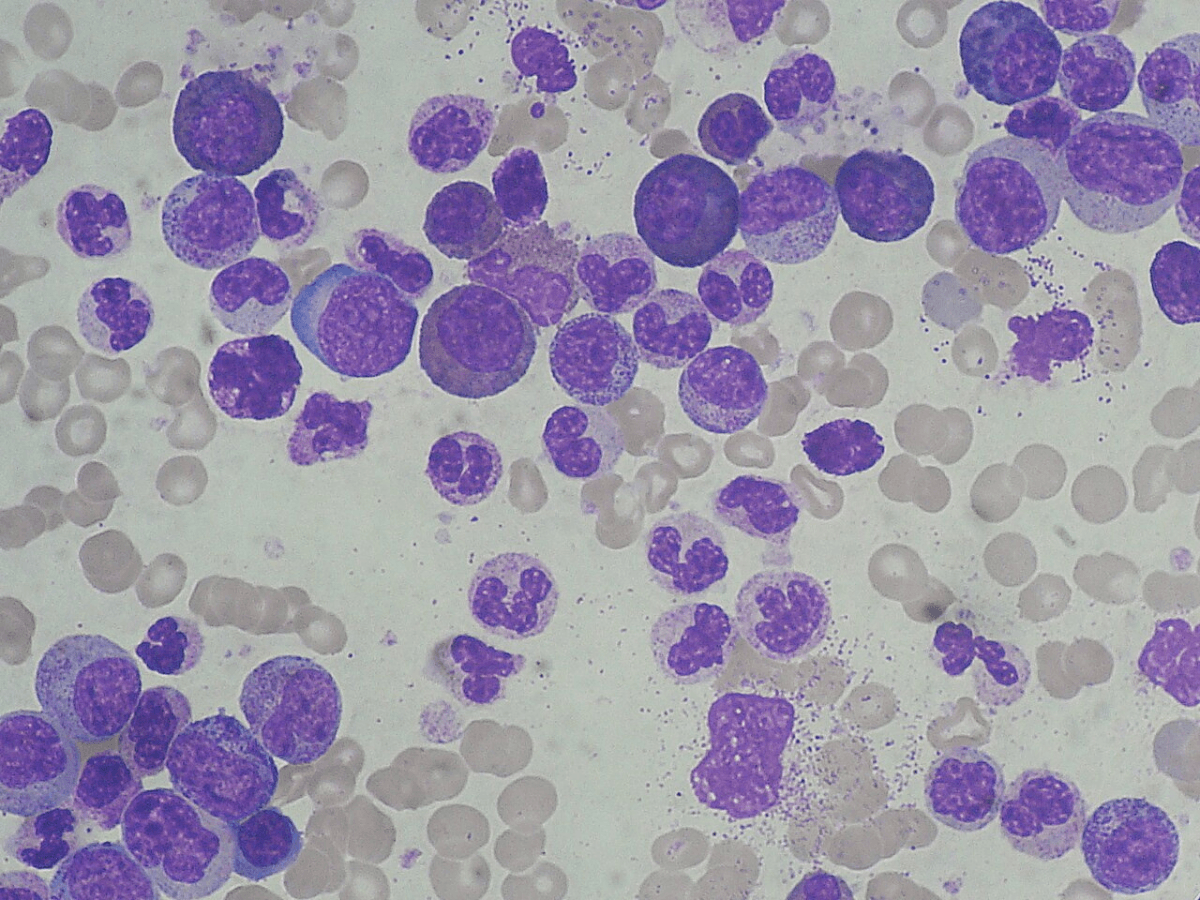
Myelodysplastic Syndromes (MDS) Updates
Current Challenges
- Anemia dominates lower-risk MDS patients, requiring frequent transfusions and clinic visits that impact quality of life. There are limited effective treatment options for managing cytopenia-related symptoms and morbidities.
- Established therapies include erythropoiesis-stimulating agents and lenalidomide, while newer agents like luspatercept and nematostat have been introduced. Luspatercept was approved approximately two years ago based on the COMMANDS trial comparing it to erythropoietin in transfusion-dependent patients.
New Updates
- ASCO data confirmed that luspatercept provides superior and more durable transfusion independence compared to erythropoietin, with responses lasting over 12-18 months.
- Emerging data suggest potential survival improvement with luspatercept, though the statistical methodology for this finding remains questionable.
Myeloproliferative Neoplasms - Essential Thrombocythemia
Current Challenges
- Essential thrombocythemia patients with high platelet counts need effective treatment options beyond first-line hydroxyurea, especially for those who are resistant or intolerant to it.
- Current second-line treatment with anagrelide has limited efficacy for blood count correction and symptom management.
- The standard treatment approach includes observation for low-risk patients, aspirin for intermediate risk, and hydroxyurea or anticoagulation for high-risk patients.
New Updates
- ROPEG Interferon Alpha 2B (approved for polycythemia vera) showed impressive results in ET patients, achieving the composite endpoint in over 40% versus 5% with anagrelide.
- The interferon demonstrated potential disease-modifying effects with reduced allelic burden for driver mutations and durable symptom improvement lasting over a year, though it's not technically approved for ET.
Acute Myeloid Leukemia (AML) - Menin Inhibitors
Current Challenges
- AML patients with KMT2A rearranged or NPM1 mutated leukemias have limited treatment options, particularly in relapsed/refractory settings where traditional therapies have failed.
- TP53-mutated AML/MDS patients have poor outcomes with standard Venetoclax-based therapies, showing very little benefit and mainly causing cytopenias.
- The venetoclax-azacitidine combination is standard care for older adults unfit for intensive chemotherapy, with oral hypomethylating agents like Inqovi being explored for convenience.
- Current Venetoclax-azacitidine combination therapy requires clinic visits for IV azacitidine administration and shows no cure plateau, indicating the need for additional therapeutic approaches.
New Updates
- Revumenib (menin inhibitor) was approved late last year for KMT2A rearranged or NPM1 mutated leukemias based on Augment101 trial data.
- Ziftomenib (competitor menin inhibitor) showed similar efficacy to revumenib in NPM1 mutated leukemias with 25% CR/CRH rates and median survival around 6 months, but with less QTC prolongation risk.
- Venetoclax is being studied in combination with oral azacitidine. This approach aims to provide a more convenient treatment option, especially for older patients who may have difficulty with intravenous therapies.
- Metronomic treatment with very low doses of cytarabine combined with venetoclax in patients with TP53 mutations. Preliminary results suggested that this approach might yield higher remission rates and lower toxicity compared to standard treatments.
Additional Updates on Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN)
- PVAC (Pivecimab Sunirine), a CD123 antibody-drug conjugate, showed 70-75% response rates as single-agent therapy in newly diagnosed BPDCN patients.
- PVAC demonstrated better tolerability than approved Tagraxofusp, avoiding capillary leak syndrome while causing manageable peripheral edema and cytopenias.
Key Takeaways
The ASCO meeting reinforced confidence in established therapies while highlighting emerging treatment paradigms across hematologic malignancies. For MDS, luspatercept's durability data provides reassurance that clinicians are using an agent with sustained long-term benefits, extending well beyond the initial approval studies. The intriguing interferon data for essential thrombocythemia patients suggests a potential disease-modifying approach that could reshape treatment algorithms for this condition.
The AML landscape is rapidly evolving with menin inhibitors establishing themselves as a significant new drug class. With revumenib already approved for KMT2A rearranged and NPM1 mutated leukemias, and ziftomenib showing comparable efficacy data, the field is becoming increasingly competitive. Both agents demonstrate similar response rates of 20-25% with several months of durability, though ziftomenib may offer advantages with reduced QTC prolongation risk compared to revumenib's notable cardiac toxicity profile.
Venetoclax-based therapies continue their expansion across multiple treatment settings, with the oral azacitidine combination representing a particularly meaningful advance for patient convenience and quality of life. The ability to achieve equivalent outcomes to IV-based regimens while eliminating clinic visits for infusions could substantially improve the treatment experience for older AML patients. Additionally, the metronomic approach for TP53-mutated patients offers hope for a historically challenging population, potentially providing better outcomes with reduced toxicity through a differentiation-based mechanism rather than traditional cytotoxic approaches.
Finally, rare malignancies like BPDCN may soon benefit from more effective and tolerable treatment options, with PVAC's impressive single-agent activity and improved safety profile compared to existing therapies potentially transforming outcomes in this difficult-to-treat disease.