The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
President Joe Biden’s Prostate Cancer Diagnosis: Can It Be Cured?
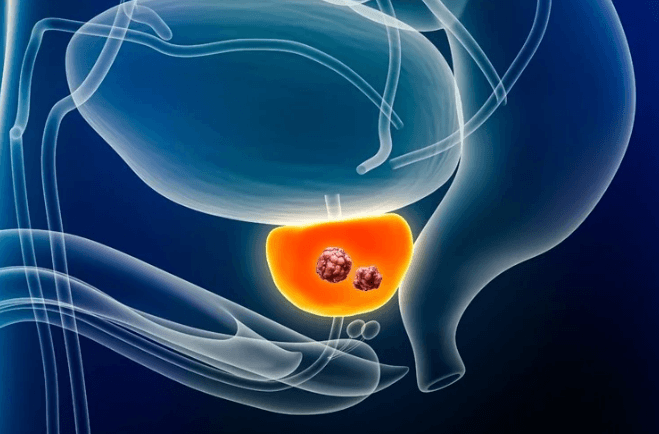
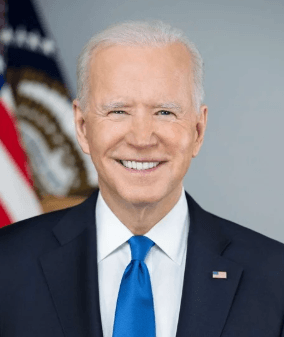
On Sunday, May 18, 2025, the office of former President Joseph R. Biden Jr. disclosed that he has been diagnosed with an aggressive form of prostate cancer that has spread to his bones. The diagnosis followed a routine physical exam during which a small nodule was found in his prostate, prompting further evaluation. While in office, Mr. Biden had cancerous lesions removed from his chest and underwent Mohs surgery to remove several non-melanoma skin cancers. Given his history of cancer, could this latest diagnosis have been prevented?
The American Cancer Society estimates that 313,780 new prostate cancer cases will be reported in 2025, with 35,770 deaths. There was a sharp decline in the number of cases diagnosed between 2007 to 2014 due to fewer men being screened as a result of changes in recommendations. Since 2014, new cases of prostate cancer have been rising by about 3% each year. Based on data from 2018 to 2022, roughly 1 in 8 men (12.9%) will be diagnosed with prostate cancer during their lifetime. By 2022, around 3.5 million men in the U.S. were living with the disease. Could earlier warning signs have helped reduce these numbers?
Risk Factors Of Prostate Cancer
One well-established risk factor for prostate cancer is advancing age, which likely played a role in Mr. Biden’s case. Prostate cancer is more commonly diagnosed after the age of 50. Age-related factors such as a declining immune response, changes in cholesterol metabolism, reduced testosterone levels, and genetic and epigenetic changes have all been strongly linked to the risk of developing prostate cancer.
Other notable risk factors include ethnicity (Black race), certain genetic mutations, insulin-like growth factors, and family history. Lifestyle factors such as diet, tobacco and alcohol use, obesity, and physical inactivity may also raise the risk of developing prostate cancer. In addition, environmental exposures, including contact with certain chemicals or ionizing radiation, have been linked to increased risk.
Can Prostate Cancer Be Prevented?
While some risk factors for prostate cancer, such as age or genetics, cannot be changed, others related to lifestyle, diet, and environment are modifiable. According to the World Health Organization (WHO), 30 to 50% of all cancers can be prevented by adopting healthy lifestyle choices. Research shows that diets rich in anti-cancer compounds, found in foods like cruciferous vegetables, tomatoes, soy, and green tea, are associated with a reduced risk of prostate cancer. Conversely, lowering the intake of trans and saturated fats may help prevent the disease, as these fats contribute to conditions that drive prostate cancer development.
Maintaining a healthy weight is also important. Because elevated insulin levels are a risk factor, regular exercise can help by reducing inflammation, boosting immune function, and counteracting the harmful effects of a sedentary lifestyle. Quitting smoking, drinking alcohol in moderation, and ensuring adequate vitamin D levels may also offer protective benefits against prostate cancer.
Can Prostate Cancer Be Found Early?
Prostate cancer can range from a slow-growing, non-aggressive disease that may not require treatment to a fast-developing, aggressive form. Screening typically involves measuring prostate-specific antigen (PSA) levels in the blood (with levels above 4.0 ng/mL often raising concern) and performing a digital rectal examination (DRE).
However, PSA tests are not always accurate. They can yield false-positive results, leading to unnecessary and often uncomfortable biopsies. False-negative results are also possible, potentially giving men a false sense of reassurance. Because of these uncertainties, it remains unclear whether the benefits of routine screening outweigh the risks.
The United States Preventive Services Task Force (USPSTF) recommends that men aged 55 to 69 make individual decisions about PSA-based screening in consultation with their clinician. This shared decision-making should consider factors such as family history, race or ethnicity, existing health conditions, personal values, and preferences regarding potential screening and treatment outcomes. The USPSTF advises against screening men who do not express a clear preference for it.
For men aged 70 and older, the USPSTF recommends against routine PSA-based screening for prostate cancer. In Mr. Biden’s case, based on these recommendations and his previously released medical records, there appeared to be no clinical indication for prostate cancer screening at the time. His diagnosis followed unspecified urinary symptoms, underscoring that cancer can sometimes develop unexpectedly and progress rapidly.
What Are The Treatment Options For Metastatic Prostate Cancer?
Mr. Biden’s cancer is “characterized by a Gleason score of 9 with metastasis to the bone,” indicating Stage 4 disease that has spread beyond the prostate. According to a statement from Mr. Biden’s office, “while this represents a more aggressive form of the disease, the cancer appears to be more hormone-sensitive, which allows for effective management.”
The clinical management of prostate cancer varies depending on the stage and progression of the disease. For localized cancer, the standard treatment is definitive therapy with either surgical removal of the tumor through a procedure known as radical prostatectomy, which involves the complete removal of the prostate gland, or radiation therapy to the prostate. Additionally, depending on the presence of high-risk pathologic features of the tumor, short-term androgen deprivation therapy (ADT) can also be added to definitive therapy.
In cases where prostate-specific antigen (PSA) levels remain elevated after surgery but there is no evidence of cancer spread, hormone-based treatments are commonly used. This typically includes ADT in combination with androgen receptor signaling inhibitors (ARSIs). These therapies work by lowering levels of male hormones (androgens) that fuel prostate cancer growth.
For advanced or metastatic prostate cancer—particularly when the cancer has spread to the bones, as in Mr. Biden’s case—treatment options broaden to include bisphosphonates, denosumab, corticosteroids, radiation therapy, radiopharmaceuticals, ablative treatments, surgery, and medications to manage pain. Additional therapies such as chemotherapy, targeted therapy, and immunotherapy may also be used to help control disease progression and improve quality of life.
Conclusion
After receiving an outpouring of love and support from around the world following the disclosure of his diagnosis, Mr. Biden shared in a social media post: “Cancer touches us all. Like so many of you, Jill and I have learned that we are strongest in the broken places. Thank you for lifting us up with love and support.
Author

Dr. Jordan Ciuro is an Assistant Professor of Medicine and Medical Oncologist with a specialization in genitourinary at Emory Winship Cancer Institute in Atlanta, Georgia. Early in her training, she discovered her passion for medicine and helping vulnerable patient populations, which led her to the AUC School of Medicine, where she completed her medical school training with honors. She then completed her Hematology Oncology Fellowship at Ascension Providence Hospital, Michigan State University, as Chief Fellow. Here, she also completed her Internal Medicine Residency as Chief Resident. She is currently the lead physician preceptor in the fellow’s oncology clinic at Grady Memorial Hospital and has a passion for teaching and mentoring aspiring students who are underrepresented in the health community. Her interests include writing investigator-initiated trials focusing on healthcare disparities and geriatric survivorship to tailor therapy to reduce toxicity and improve patient outcomes and disparities in solid oncology.