The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
Melanoma Monday 2025: On Skin Cancer Prevention & Awareness
 Expert insights from Dr. Shailender Bhatia
Expert insights from Dr. Shailender Bhatia
Introduction
Do you know that Melanoma accounts for 1% of all skin cancers, yet causes over 80% of skin cancer deaths?
Melanoma Monday falls on the first Monday of May and kicks off National Melanoma Month, an awareness campaign dedicated to educating the public about this serious form of skin cancer. Established in 1995 by the American Academy of Dermatology (AAD), Melanoma Monday aims to improve understanding and promote prevention. So, how can melanoma be prevented, and what steps can individuals take to protect themselves? Let us mark Melanoma Monday by learning more about melanoma and effective ways to reduce individual risk.
What is Melanoma?
The skin is the largest organ of the human body and protects against physical, chemical, and biological agents. Melanoma is characterized by the uncontrolled growth of melanocytes, melanin (pigment) producing cells in the skin. This aggressive disease can be classified into different clinical subtypes that differ in presentation, demographics, and molecular profile. Based on appearance and growth, there are six types of melanoma: Superficial spreading melanoma, Nodular melanoma, Acral-lentiginous melanoma, Lentigo maligna melanoma, Amelanotic melanoma, and Desmoplastic melanoma. Notably, superficial spreading melanoma(SSM) represents approximately 70% of all melanomas. This form of skin cancer can be found on all body surfaces, especially the trunk of males.
Melanoma develops in five stages. In Stage 0, the cancer is confined to the top layer of the skin (the epidermis) and has not spread. In Stages 1 and 2, the melanoma remains in the skin but becomes thicker and may show signs of increased risk. By Stage 3, the cancer has spread to nearby lymph nodes. In Stage 4, melanoma has metastasized to distant parts of the body, such as other organs or lymph nodes farther from the original site.
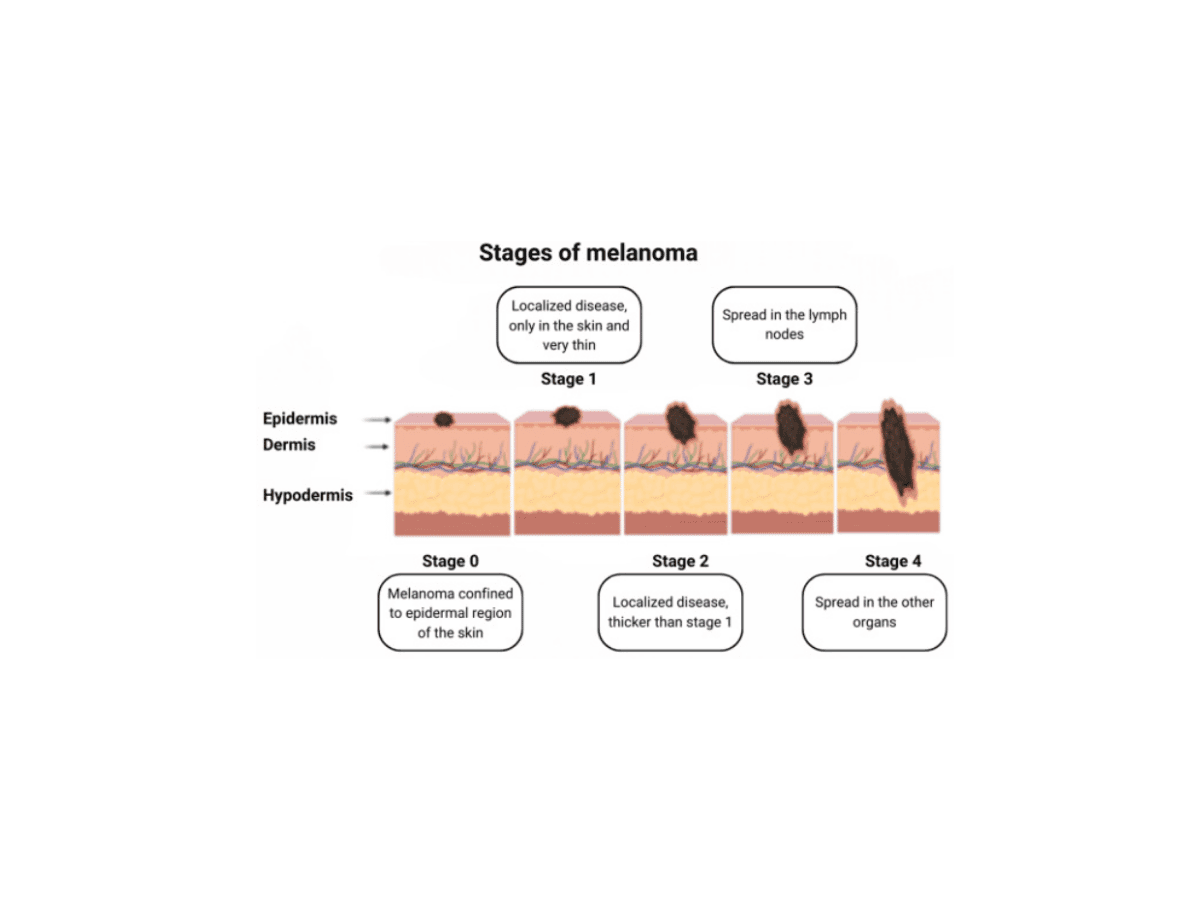 Image by Roky et al., 2024
Image by Roky et al., 2024
Expert Insights with Dr. Shailender Bhatia
Dr. Bhatia is the director of the melanoma and renal cancer team at Fred Hutchinson Cancer Center. In recognition of Melanoma and Skin Cancer Awareness Month, he shares a brief message with the broader public. He stated:
“The most important part of addressing skin cancer is prevention. Being vigilant about sun exposure and consistently using sun protection measures is key. It is also important to regularly visit your dermatologist and stay aware of any changes on your skin— It is your largest organ, after all.
At the same time, there is some reassurance in knowing that significant advances have been made in treating skin cancers, especially when they become more advanced or aggressive, like melanoma or Merkel cell carcinoma. We can feel confident in the treatment options available today, even if a skin cancer diagnosis does occur.”
How Common is Melanoma?
In 2025, the American Cancer Society estimates that about 104,960 new cases of melanoma will be diagnosed in the U.S., leading to approximately 8,430 deaths. Globally, around 330,000 new melanoma cases were reported in 2022, with nearly 60,000 deaths. Melanoma and other skin cancers are more common in people with lighter skin, so rates of occurrence vary depending on the region. Melanoma is the 17th most common cancer and the 23rd leading cause of cancer death worldwide. Europe has the highest number of cases, accounting for 46.4% of global incidence, followed by North America at 32.4%. Europe also has the highest number of deaths from melanoma (46.2%), with Asia following at 21%.
Risk of Getting Melanoma
A well-known risk factor for melanoma is sun exposure, particularly ultraviolet (UV) radiation from the sun. The impact of UV exposure on transforming normal skin cells into cancerous ones depends on several factors, including an individual’s genetics, melanin levels, and the specific wavelengths of UV light. UV radiation has been shown to cause errors in DNA replication, which can lead to uncontrolled cell growth and, ultimately, cancer. Some of these errors commonly affect key proteins that regulate cell growth and differentiation, such as NRAS and BRAF.
In addition to sun exposure, other risk factors for melanoma include indoor tanning, immunosuppression, moles, family history, and obesity. Having a parent, sibling, or child who has had melanoma increases the risk of developing the disease. A 2020 economic analysis projected that banning indoor tanning for individuals aged 35 and under could prevent approximately 448,000 melanoma cases, due to the high levels of UV radiation associated with tanning beds. Similarly, studies have shown that immunosuppressed individuals, such as those with HIV, are at increased risk for melanoma. Moles, or nevi, benign growths of melanocytes, are also considered precursors and markers for elevated melanoma risk. As for obesity, excess body fat has been linked to genetic mutations that may drive melanoma development.
Prevention Measures
According to the Centers for Disease Control and Prevention (CDC), the best way to reduce the risk of skin cancer is to make sun safety part of your daily routine and avoid both indoor tanning and sunbathing. Since many outdoor environments are not designed with sun safety in mind, using proven protection strategies, such as seeking shade, wearing hats and sunglasses, and applying sunscreen, is a great first step in the right direction. The American Cancer Society recommends avoiding the sun between 10 a.m. and 4 p.m. when ultraviolet (UV) rays are strongest. If that is not possible, wearing protective clothing and using a broad-spectrum sunscreen with an SPF of 30 or higher is advised.
Public health initiatives have also shown success in preventing skin cancer. For example, the SunWISE program by the National Environmental Education Foundation is a free K–8 environmental and health education initiative that teaches children about sun safety, UV radiation, and the ozone layer. It has been estimated to prevent more than 11,000 skin cancer cases and 50 related deaths. Similarly, Australia's SunSmart program uses mass media, including television campaigns, to promote sun protection behaviors. On a biological level, eumelanin, the type of melanin more commonly produced in dark-skinned individuals, offers greater protection against UV radiation than pheomelanin, present in light-skinned individuals.
When it comes to screening, a visual skin examination is the most commonly used method. This can be done by simply looking at the skin or with a magnifying tool called a dermatoscope. Clinicians often use the “ABCDE” rule to identify potential melanomas. “A” stands for asymmetry—one half of a mole looks different from the other. “B” is for border—melanomas often have uneven or notched edges. “C” stands for color—moles with multiple colors or shades are more concerning. “D” is for diameter—melanomas are usually larger than 6 millimeters (about the size of a pencil eraser). “E” is for evolution—any changes in size, shape, or color over time. If a suspicious lesion is found, a biopsy is needed to confirm whether it is cancerous.
Despite these tools, the U.S. Preventive Services Task Force (USPSTF) has stated that there is not enough evidence to determine whether routine visual skin exams by clinicians do more good than harm. The task force is calling for more research to better understand the benefits and risks of such screenings.
Current Treatments
Unlike other cancers, melanoma has an increased 5-year relative survival of 94%, owing to early diagnosis and incidental detection. A host of new treatment approaches, such as immunotherapy and targeted therapy, have contributed to the improved outcomes for melanoma. However, its incidence continues to increase.
Treating melanoma often involves a combination of approaches, depending on how advanced the cancer is. Most commonly, treatment begins with surgery to remove the tumor and some surrounding tissue. After surgery, some patients receive additional treatments like chemotherapy or radiation to help reduce the risk of the cancer coming back. For more advanced melanoma, newer treatments like immunotherapy and targeted therapy are often used. These treatments help the immune system fight cancer or attack specific cancer cells more directly.
Throughout the treatment process, follow-up care is important. Regular check-ups and scans help doctors track how well the treatment is working and catch any signs that the cancer might return. Although treatment can come with side effects, it also offers hope, especially as research continues to improve the way melanoma is treated.
Conclusion
Melanoma Monday is a special day that kicks off the broader observance of Skin Cancer Awareness Month. It serves as a reminder to take care of your skin by learning about warning signs and prevention. On this day, practice sun safety, perform skin self-exams, get checked, educate others, and support the SPOT Skin Cancer program by the American Academy of Dermatology Association. Together, we can work toward a world where skin cancer is eliminated.
Works Discussed
Siegel, R. L., Kratzer, T. B., Giaquinto, A. N., Sung, H., & Jemal, A. (2025). Cancer statistics, 2025. CA: a cancer journal for clinicians, 75(1), 10–45. https://doi.org/10.3322/caac.21871
Roky, A. H., Islam, M. M., Ahasan, A. M. F., Mostaq, M. S., Mahmud, M. Z., Amin, M. N., & Mahmud, M. A. (2024). Overview of skin cancer types and prevalence rates across continents. Cancer pathogenesis and therapy, 3(2), 89–100. https://doi.org/10.1016/j.cpt.2024.08.002
Saginala, K., Barsouk, A., Aluru, J. S., Rawla, P., & Barsouk, A. (2021). Epidemiology of Melanoma. Medical Sciences, 9(4), 63. https://doi.org/10.3390/medsci9040063
PDQ® Adult Treatment Editorial Board. (2025, April 25). Melanoma treatment (PDQ®)–Patient version. National Cancer Institute. https://www.cancer.gov/types/skin/patient/melanoma-treatment-pdq