The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
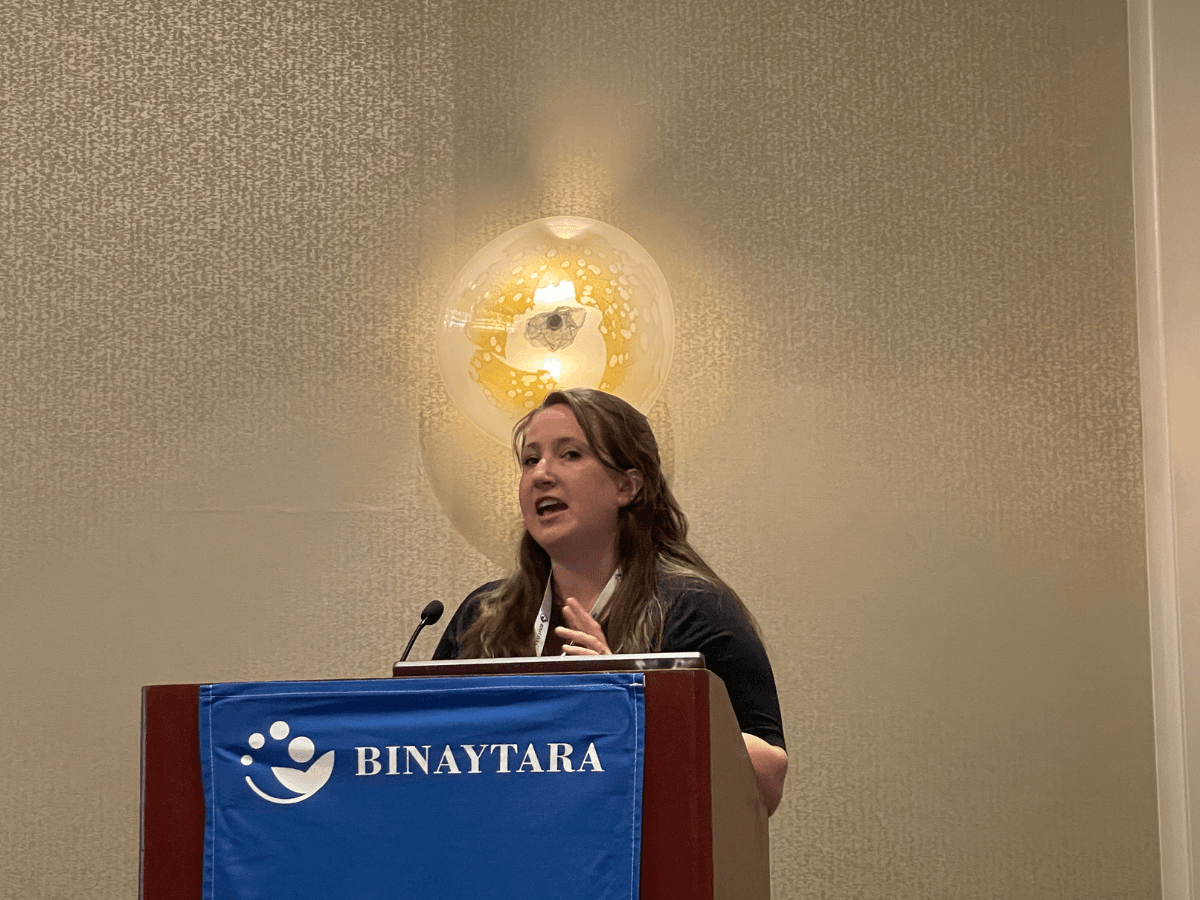
Dr. Emily N. Palmquist on De-escalation of Axillary Surgery in Early-Stage Breast Cancer
De-escalation of axillary surgery is reshaping the management of early-stage breast cancer. At the Best of Hematology and Breast Cancer conference, Dr. Emily N. Palmquist of Fred Hutchinson Cancer Center reviewed key evidence from the SOUND, INSEMA, and BOOG trials, outlining which carefully selected patients may safely omit sentinel lymph node biopsy without compromising oncologic outcomes.
At the Best of Hematology and Breast Cancer conference, Dr. Emily N. Palmquist of Fred Hutchinson Cancer Center presented on the evolving approach to axillary management in early-stage breast cancer, focusing on when sentinel lymph node biopsy can be safely omitted without compromising outcomes. Drawing on evidence from three major trials—SOUND, INSEMA, and BOOG—the presentation emphasized careful patient selection and multidisciplinary decision-making in this era of surgical de-escalation.
The transcript below has not been reviewed by the speaker and may contain errors.
Evolution of Breast Cancer Treatment
The evolution of breast cancer treatment has come a long way from compulsive mastectomy to adding options for breast reconstruction. Chemotherapy and systemic adjuvant options have exploded with many different medications. On the surgical side, the field has moved from radical mastectomy and axillary node dissection to considering breast conservation, breast reconstruction, and sentinel lymph node biopsy. The trend continues toward more systemic therapy options but possibly less local therapy.
Historical Perspective on Axillary Management
Looking specifically at the axilla, the field initially favored axillary dissection to achieve local control. Ultimately, studies showed that this didn't really offer a survival benefit. With several trials over the years, sentinel lymph node biopsy has been incorporated for clinically node-negative patients, then expanded to those who convert to clinical node negative after chemotherapy, allowing these patients to avoid more extensive nodal disease treatment. The question now is whether sentinel lymph node biopsy can be omitted altogether in select patients.
The management of the axilla in breast cancer has always been challenging. This is where tumor boards often have heated debates. It's important to discuss who can benefit from the de-escalation of axillary management surgically.
The Role of Sentinel Lymph Node Biopsy
Prior research shows that sentinel biopsy is important for staging, prognosis, and possibly helping guide some adjuvant treatment, but it doesn't really offer a survival benefit. When considering omitting this procedure, careful thought is needed about who are the correct patients are, because this decision may affect other treatment decisions.
Choosing Wisely Recommendations
Choosing Wisely recommendations came out in 2016 for routinely omitting sentinel lymph node biopsy in individuals over the age of 70 with hormone receptor-positive early-stage breast cancer. Most recently, the NCCN came out with this being a quality measure for tracking to ensure that patients who fall into this Choosing Wisely cohort are indeed having the procedure omitted. The question becomes whether this is the only route for omitting sentinel lymph nodes or if there are other candidates.
The SOUND Trial
The SOUND trial examined omission of sentinel lymph node biopsy with a primary outcome of five-year distant disease-free survival. All patients were undergoing breast conservation and were clinically node-negative, meaning they had both clinical exam without palpable adenopathy and an axillary ultrasound. If there were any abnormal nodes, those nodes had to undergo biopsy, and if they were confirmed negative, patients could be enrolled.
The trial only allowed clinical T1 tumors. Patients were randomized to either no axillary surgery or standard of care sentinel lymph node biopsy. The study allowed several subtypes of cancer in patients over age 40. Overall, the majority were postmenopausal with small tumor size just over one centimeter, nearly all being ER-positive or hormone receptor-positive, HER2-negative, grade one or two, and low Ki-67. They did allow neoadjuvant therapy in about eight patients.
The INSEMA Trial
INSEMA had a similar design but with a primary outcome of five-year invasive disease-free survival. Again, patients had breast conservation, were clinically node-negative with axillary ultrasound, but the trial allowed clinical T2 tumors. Patients were randomized one to four to no axillary surgery versus standard of care sentinel lymph node biopsy.
Despite allowing larger tumors up to clinical T2, the population remained very favorable: majority postmenopausal with small tumors, hormone receptor-positive, grade one or two, with small numbers of basal-like triple-negative disease.
The BOOG Trial
The most recent published trial was BOOG (or POSNOC), with a primary outcome of five-year regional recurrence-free survival. Again, the same sort of population was studied, allowing T1 and T2 tumors. Patients had to have an axillary ultrasound and were randomized to no axillary surgery versus sentinel node biopsy. This also represented a very favorable cohort.
Common Features Across Trials
Looking at all three trials together, they represented a very similar favorable group of patients. An important note about the assessment of the axilla is that all of these patients were planned to have whole breast radiation and were undergoing lumpectomy with whole breast radiation.
Exclusion criteria involved any multifocal, multicentric, bilateral disease, or history of prior breast cancer. The trials had slightly different five-year primary outcomes.
Patient Characteristics and Nodal Positivity Rates
These were favorable patients: clinical T1, majority grade one and two, majority hormone receptor-positive. Among those randomized to sentinel node biopsy, positive nodes were found in under about 15% across all studies, hovering between 13 to 15%. Much of that was micrometastatic disease, but a small proportion had true pathologic positivity at around 10% between the three trials.
Trial Outcomes
Local-Regional Recurrence
Local-regional recurrence was low among all these trials, which is not surprising when selecting a very favorable patient population. Local-regional recurrence hovered around 1%, and there was no difference between those who underwent sentinel biopsy versus those who underwent no axillary surgery.
Distant Recurrence
Looking at distant recurrence, again in this very favorable population, rates were around 2% across the board with no difference between those who underwent axillary surgery or not.
Overall Survival
Overall death rates were low with no difference between the two groups.
Axillary Recurrence
Axillary recurrence was very low across the board, under about 1%, and there were no differences between those who had axillary surgery or not.
Primary Endpoint Results
Looking at all three trials together with their primary endpoints, the confidence intervals between axillary surgery and not overlapped, and there was no difference. The conclusion was that omission of sentinel lymph node biopsy was not inferior to the standard of care sentinel lymph node biopsy.
Impact on Adjuvant Treatment Recommendations
Many had questions about how this would affect adjuvant treatment recommendations, as nodal status can be important.
SOUND Trial Adjuvant Therapy
In SOUND specifically, adherence to endocrine therapy was exceptional, which is probably not reflective of real-life scenarios. The use of chemotherapy was not different between the two cohorts at around 20% and 18%. The radiation standard was whole breast, although there was a subset that had atypical radiotherapy with no difference between the two groups.
INSEMA Trial Adjuvant Therapy
In INSEMA, adherence to endocrine therapy was very high at 95% with no difference between the two groups. Adjuvant chemotherapy was slightly higher in the sentinel lymph node biopsy group, which was statistically significant, but overall numbers were still quite low at 12% and 10%.
BOOG Trial Adjuvant Therapy
In BOOG, adherence to endocrine therapy was actually much lower but again not different between those who had a sentinel lymph node biopsy or not. Chemotherapy use was not statistically different. Adjuvant chemotherapy was not different. They did look at a subset of patients—everyone had breast radiation—but looking at patients guided into regional nodal radiation, there was slightly higher use of regional radiotherapy in those who had undergone sentinel lymph node biopsy.
Current Practice Guidelines
How should practice change with all this data? This is very much a multidisciplinary decision. Consideration must always be given to how decisions in the OR will affect colleagues in radiation and medical oncology.
After this data was released, a group approach was developed for offering omission of sentinel lymph node biopsy, broken into age groups to help guide decisions, because there are differences in implications for adjuvant treatment.
Postmenopausal Women Age 50-64
For postmenopausal women between age 50 and 64 who are clinical T1, hormone receptor-positive, the recommendation is limited to invasive ductal carcinoma (not lobular), grade one or two. They must be planning breast-conserving surgery with negative axillary imaging (both clinical exam and ultrasound). The plan should be for adjuvant breast radiation therapy and endocrine therapy. If all these criteria are met, omission can be offered after discussion.
Women Age 65-70
For the 65 to 70 age group, criteria include clinical T1, hormone receptor-positive ductal carcinoma, grade one to two, undergoing breast-conserving surgery. Axillary ultrasound should be performed. If there's an abnormal node and biopsy shows it's benign, patients are still eligible. They should be planning breast radiotherapy. Partial breast radiation is allowed for these patients who are otherwise eligible, and omission of radiotherapy can be considered based on PRIME II and other studies if they agree to adhere to endocrine therapy.
Women Over Age 70
For patients over 70, these trials did not affect that population. Choosing Wisely guidelines should still be followed for the omission of sentinel biopsy for early-stage hormone receptor-positive breast cancer. This is not restricted to invasive ductal carcinoma—lobular subtypes are acceptable. Dedicated axillary imaging is not required if patients are clinically node-negative on exam. Omission of radiotherapy is acceptable if they are adhering to endocrine therapy versus whole breast radiation.
When to Return to Surgery
For patients who do not want to take endocrine therapy, returning to the OR for sentinel biopsy should be considered if certain features emerge: upgrade to high grade, upstaging to a larger tumor, mastectomy required for positive margins, or surprising pathology. For younger patients who decline radiation, returning for a sentinel node biopsy should be discussed to possibly change treatment recommendations.
Future Directions and Considerations
With all this de-escalation discussed today, patient selection is huge. When favorable disease patients are selected, they do favorably. Care must be taken with how much the criteria are expanded, especially for triple-negative and HER2-positive patients, where nodal status is highly influential on other treatment recommendations.
The surgeon's job regarding the axilla is often not to save lives but to help guide what other treatments might be needed. Good communication with patients about what these decisions could affect is essential.
It will be interesting to see how this evolves. In these studies, radiation was whole breast for everyone. But with the move toward partial breast radiation, is whole breast radiation somehow a replacement for axillary surgery or lymph node surgery? The implications for systemic therapy decisions and colleagues are really important.
As indications for certain treatments expand and are often linked to nodal status, ongoing discussions about what that might mean are necessary. For most hormone receptor-positive breast cancer patients, the trajectory is long and recurrences can happen late. Following these patients longer is important to truly see if there is any difference in the future.
Balancing De-escalation with Patient Safety
As de-escalation continues, the question must always be asked: Do we ever go too far? As a surgeon, it's important to remember that while every time you cut it's not necessarily a cure, every time you cut, you can hurt someone too. Balancing those two considerations together is essential.