The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
Lung Cancer 101: A Complete Guide to Risks, Symptoms, Diagnosis, and Treatment
Lung cancer remains the leading cause of cancer death worldwide, but advances in early detection, screening, and personalized treatments—including immunotherapy, molecular testing, and targeted therapies—are transforming outcomes for many patients. This introductory guide explains the types of lung cancer, key symptoms, risk factors, prevention strategies, disparities, and modern treatment options.
Lung cancer remains the leading cause of cancer-related deaths worldwide and in the United States. But remarkable progress in prevention, early detection, and treatment has been made, shifting the outcomes for many patients. Once considered a uniformly fatal disease, lung cancer is now increasingly treatable, especially when detected early or guided by molecular testing.
What Is Lung Cancer?
Lung cancer occurs when abnormal cells in lung tissue grow uncontrollably, forming tumors that can invade nearby or distant organs. These tumors commonly arise from the bronchi, bronchioles, or alveoli and are classified based on the type of cell in which the disease begins. Lung cancer often spreads to structures like the brain, bones, liver, lymph nodes, and adrenal gland. Lung cancer development is complex and can occur due to multiple factors. It can occur due to several genetic changes that activate tumor growth pathways and block tumor-suppressing pathways. As a result, the accumulation of many genetic and epigenetic changes over a long period causes weakened DNA, uncontrolled cell division, and eventually the initiation of lung cancer.
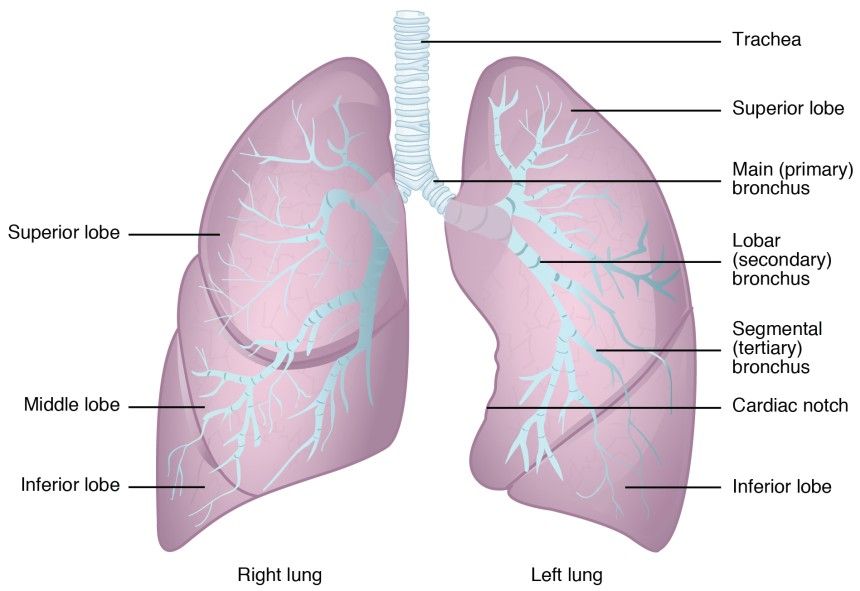
The gross anatomy of the lung
Types of Lung Cancer
Lung cancers are broadly classified into two types, based on cell appearance under the microscope and their biological behavior: Non-small cell lung cancer (NSCLC) and Small cell lung cancer (SCLC).
Non–Small Cell Lung Cancer (NSCLC)
NSCLC accounts for roughly 80–85% of all lung cancers and generally grows and spreads more slowly than SCLC. Within NSCLC, three major subtypes are recognized:
Adenocarcinoma: The most common subtype, making up about 45% of all lung cancers according to a 2022 study. It originates in mucus-producing cells in the outer parts of the lungs and is more frequently seen in women, non-smokers, and younger adults. Advances in targeted therapies have significantly improved survival for adenocarcinoma patients with EGFR, ALK, or KRAS mutations.
Squamous Cell Carcinoma: Arises from thin, flat cells lining the lung’s airways, often linked to a history of smoking. It typically occurs near the center of the lungs and accounts for roughly 20–25% of cases. Symptoms such as coughing up blood or airway obstruction may appear earlier in this subtype.
Large Cell Carcinoma: A less common and more aggressive variant that can begin in any region of the lungs. It tends to grow and metastasize faster than adenocarcinoma or squamous cell carcinoma. With the improvement of molecular diagnostics, fewer cancers today are classified as large cell carcinoma because they are reclassified into more precise subtypes.
Small Cell Lung Cancer (SCLC)
SCLC is the most aggressive tissue subtype of lung cancer, representing about 13–15% of all cases. It often originates in the neuroendocrine cells of the lungs and is strongly associated with tobacco exposure. It tends to grow rapidly and metastasize early. Over two-thirds of patients who present with SCLC at the clinic are already at an advanced stage.
SCLC has two main patterns:
Small Cell Carcinoma: The classic, high-grade neuroendocrine cancer most often treated with systemic therapy.
Combined Small Cell/Non-Small Cell Carcinoma: Contains features of both histologies and may respond differently to standard regimens.
Rare Lung Cancer Types
Carcinoid Tumors: Slow-growing neuroendocrine tumors are often diagnosed incidentally.
Sarcomatoid Carcinomas and Pulmonary Blastomas: Rare, aggressive cancers requiring molecular testing for appropriate classification.
As diagnostic technology improves, more lung cancers are identified by their molecular profile, allowing oncologists to personalize treatment based on genetic mutations and growth patterns.
Symptoms of Lung Cancer
Common lung cancer symptoms observed when patients first present to the clinic include cough, shortness of breath, pain, and weight loss. Cough is particularly common, occurring in 50–75% of lung cancer patients, and is often seen in those with squamous cell or small cell carcinomas. Patients may also experience dull, aching, and persistent chest pain, typically on the same side as the primary tumor.
When the cancer has spread, additional symptoms can arise depending on the site of metastasis: bone metastases may cause pain in the back, chest, or extremities; adrenal gland involvement can lead to nausea, abdominal pain, and weakness; and brain metastases may result in neurological dysfunction. Other systemic or non-specific symptoms can include fatigue, fever, and swollen lymph nodes.
Lung Cancer Risk Factors
Tobacco smoking remains the primary cause of lung cancer, responsible for about 80% to 90% of all cases. Smokers have roughly a 20 times greater risk of developing lung cancer compared to non-smokers. Other risk factors include exposure to secondhand smoke, use of, cigars, pipes, water pipes, as well as environmental exposures such as radon and asbestos. Certain medical conditions, like asthma, pneumonia, tuberculosis, COPD, emphysema, chronic bronchitis, and HIV, can also increase susceptibility. Despite ongoing efforts to reduce tobacco use, lung cancer rates remain high.
Some risk factors, however, are beyond personal control, including older age (65 and above), family history, inherited gene mutations, and prior radiation therapy to the chest. Considering these unchangeable risks and the continued exposure to carcinogenic air pollutants, what preventive measures can be implemented to help reduce the likelihood of developing lung cancer?
Can Lung Cancer Be Prevented? Tips for Early Detection and Risk Reduction
Quitting smoking is the most important step you can take to prevent lung cancer. Public health efforts to help people stop smoking have already led to fewer cases, and the benefits continue even after a diagnosis. For those undergoing lung cancer treatment, quitting smoking can improve survival, reduce complications after surgery, and make therapies like chemotherapy and radiation more effective.
Early detection can improve lung cancer survival by 20% to 33%, depending on the population studied. This highlights the importance of staying informed and raising awareness about screening methods to enhance survival and overall patient outcomes.
According to the American Cancer Society (ACS) lung cancer screening guidelines, it is recommended that an annual lung cancer screening be done with low-dose computed tomography (LDCT) for adults aged 50–80 who currently smoke or have quit and have a 20+ pack-year smoking history, meaning the equivalent of smoking one pack per day for 20 years.
LDCT combines a computer with an X-ray machine to deliver a very low dose of radiation while producing detailed images of the body’s internal structures. Large clinical studies, including the U.S. National Lung Screening Trial (NLST) and the European NELSON trial, have demonstrated that LDCT screening can reduce lung cancer deaths by roughly 20% to 30%. Despite proven benefits, screening rates remain low, particularly among underserved communities.
Lung Cancer Treatment: Options, Advances, and What to Expect
Thanks to advances in therapy and early detection, the overall five-year survival rate of lung cancer has improved to around 30%, with localized lung cancer being about 60%, regional about 35%, and distant about 10%. This means that each percentage of patients at their respective stages have not died from their cancer 5 years later.
Treatment for non-small cell lung cancer (NSCLC)
Recent innovations in NSCLC therapy have been transformative. Patients’ treatment largely depends on the stage of the tumor and is divided into early(stage 1-2), locally advanced (stage 3), and metastatic(stage 4 lung cancer).
For early stages (stage 1 or 2), most patients are treated with surgery to remove the tumor. In some cases, chemotherapy or immunotherapy may be recommended before or after surgery to lower the risk of cancer returning. The goal at these stages is often to cure the cancer by removing all visible disease.
For locally advanced NSCLC (stage 3), treatment usually involves a combination of therapies. This can include chemotherapy and radiotherapy together, and sometimes surgery if the tumor can be completely removed. Often, immunotherapy may be added after chemo-radiotherapy to help keep the cancer from coming back. The main aim is to control the disease and reduce the chance of spread.
For metastatic NSCLC (stage 4 lung cancer), when the cancer has spread to other parts of the body, most patients receive what’s called “systemic treatment.” This includes chemotherapy, targeted therapies (if the tumor has certain gene changes), and immunotherapy. Surgery is generally not used for stage 4 lung cancer, but it may be used in highly selected cases. The overall goal of treatment at this stage is to slow down the cancer’s progress, manage symptoms, and improve quality of life, instead of curing the cancer.
Every patient’s treatment is personalized based on the stage, cancer type, results of special tests on their tumor, and their overall health. New treatments like targeted therapies or immunotherapy are also becoming more common, especially for advanced stages, if certain molecular markers are present in the tumor.
Treatment for small cell lung cancer (SCLC)
Small cell lung cancer (SCLC) is usually treated in different ways based on how much it has spread at diagnosis.
1. Limited Stage SCLC. This describes cancer only in one lung and nearby lymph nodes. Treatment often combines chemotherapy and radiation at the same time to give the best chance of a cure. Chemotherapy typically involves two medications: carboplatin (or cisplatin) and etoposide. Radiation is given to the chest at the same time as chemotherapy.
For very early and rare cases, surgery may be possible, usually followed by chemotherapy. A newer treatment, immunotherapy called durvalumab, may be added after chemo-radiation to help prevent cancer from returning.
2. Extensive Stage SCLC. This describes cancer that has spread to the other lung or further in the body. Treatment mainly uses chemotherapy, usually the same two drugs, carboplatin (or cisplatin) and etoposide. Immunotherapy drugs are now added to first-line treatment to help the immune system fight cancer. If the cancer responds well, chest radiation may be added to control the disease in the lungs.
3. Relapsed SCLC: If the cancer returns, different types of chemotherapy (topotecan, lurbinectedin, or repeat carboplatin/etoposide for patients who responded well the first time) may be used. Newer treatments like tarlatamab (a “bispecific T-cell engager” that targets cancer cells) are available for certain patients after standard treatments stop working. Other options might include clinical trials of new drugs.
Every treatment plan is tailored to each individual. Your doctor will recommend the best option based on how far the cancer has spread, your health, and other important factors.
Disparities in Lung Cancer
Lung cancer shows significant disparities in who it affects and in patient outcomes across different populations and regions.
Global and Regional Disparities
Lung cancer rates and deaths are highest in high-income regions with very high Human Development Index (HDI), such as Eastern Asia, Europe, and North America. In 2022, Eastern Asia accounted for over half of new cases and nearly half of deaths, while some African regions had much lower rates. In some areas, the risk of dying from lung cancer is up to 15 times higher than in others.
Socioeconomic Disparities
Higher HDI countries have more lung cancer cases, partly due to older populations, greater risk factors, and better diagnostics. Low- and middle-income countries (LMICs) face rising rates from limited smoking control and restricted access to healthcare and advanced treatments, leading to poorer outcomes.
Sex and Age Disparities
Men are about twice as likely as women to develop and die from lung cancer globally, with the male-to-female ratio especially pronounced in parts of Europe and Asia. Age is also a significant factor: rates increase dramatically as people get older, with most new cases and deaths occurring in those over 55 years old.
Racial, Ethnic, and Screening Disparities
In many countries, lung cancer screening and prevention efforts primarily target population groups at the highest statistical risk, often based on data from White men. However, women and racial minorities may face increased risk at younger ages or with less tobacco exposure, which can result in under-detection or later diagnosis for these populations. People of lower socioeconomic status and those belonging to racial or ethnic minorities are also less likely to be eligible for and benefit from lung cancer screening due to access barriers or strict eligibility requirements.
Without intervention, studies show that global lung cases and deaths could nearly double by 2050, with disparities persisting by geography, sex, and income. Reducing these disparities requires:
- Stronger tobacco control programs
- Early detection for all high-risk groups
- Broader access to diagnostics and effective treatments
Ask An Expert
Have questions about lung cancer? Submit them to connect with lung cancer specialists for evidence-based answers tailored to individual risk, values, and goals of care.
Share Your Story
Lived experiences help raise awareness and support others navigating screening, diagnosis, treatment decisions, and survivorship in lung cancer communities. Interested in sharing your journey? Share your story here.
More Resources
Learn More About What Lung Cancer Experts Are Saying
- Lung Cancer Prevention Strategies and Latest Therapies
- How Tobacco Fuels the Lung Cancer Epidemic
- Understanding the Lung Cancer Screening Guidelines
Continuing Medical Education
- Personalized Lung Cancer Care: Updates on Efficacy, Toxicity, and Clinical Decision-Making
- Thoracic Oncology Updates from ASCO 2025
- Personalizing NSCLC Treatment: Biomarkers and Targeted Options I
- Personalizing NSCLC Treatment: Biomarkers and Targeted Options II
Top Organizations Advancing Lung Cancer Advocacy
- The International Association for the Study of Lung Cancer (IASLC)
- Lungevity
- American Lung Association
- Lung Cancer Initiative
- Lung Cancer Foundation of America: Research and Awareness
- Lung Cancer Research Foundation
Where to Find More About Lung Cancer Clinical Trials
- The National Cancer Institute
- Massive Bio
- American Lung Association
- Memorial Sloan Kettering Cancer Center
- Moffitt Cancer Center
References
- Behrouzi, R., & Blackhall, F. (2025). State of the art in treatment of small cell lung cancer. Therapeutic Advances in Medical Oncology, 17, 17588359251363518. https://doi.org/10.1177/17588359251363518
- Centers for Disease Control and Prevention. (n.d.). Lung cancer stat bite. U.S. Department of Health and Human Services. https://www.cdc.gov/united-states-cancer-statistics/publications/lung-cancer-stat-bite.html#:~:text=Table_title:%205%2Dyear%20relative%20survival%20Table_content:%20header:%20%7C,Distant%20%7C%205%2DYear%20Relative%20Survival:%209.4%25%20%7C
- Centers for Disease Control and Prevention. (n.d.). Lung cancer types. U.S. Department of Health and Human Services. https://www.cdc.gov/united-states-cancer-statistics/publications/lung-cancer-types.html
- Jeon, H., Wang, S., Song, J., Gill, H., & Cheng, H. (2025). Update 2025: Management of non-small-cell lung cancer. Lung, 203(1), 53. https://doi.org/10.1007/s00408-025-00801-x
- Lumen Learning. (n.d.). The lungs. In Anatomy and physiology II. https://courses.lumenlearning.com/suny-ap2/chapter/the-lungs/
- Mithoowani, H., & Febbraro, M. (2022). Non-small-cell lung cancer in 2022: A review for general practitioners in oncology. Current Oncology, 29(3), 1828–1839. https://doi.org/10.3390/curroncol29030150
- Moffitt Cancer Center. (n.d.). Where does metastatic lung cancer spread to? https://www.moffitt.org/cancers/lung-cancer/metastatic-lung-cancer/where-does-metastatic-lung-cancer-spread-to/
- Smolarz, B., Łukasiewicz, H., Samulak, D., Piekarska, E., Kołaciński, R., & Romanowicz, H. (2025). Lung cancer—Epidemiology, pathogenesis, treatment and molecular aspect (Review of literature). International Journal of Molecular Sciences, 26(5), 2049. https://doi.org/10.3390/ijms26052049
- Solta, A., Ernhofer, B., Boettiger, K., et al. (2024). Small cells – big issues: Biological implications and preclinical advancements in small cell lung cancer. Molecular Cancer, 23, 41. https://doi.org/10.1186/s12943-024-01953-9
- Midthun, D., (2025). Clinical manifestations of lung cancer. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-of-lung-cancer#H355282333
- Zhou, J., Xu, Y., Liu, J., Feng, L., Yu, J., & Chen, D. (2024). Global burden of lung cancer in 2022 and projections to 2050: Incidence and mortality estimates from GLOBOCAN. Cancer Epidemiology, 93, 102693. https://doi.org/10.1016/j.canep.2024.102693
Medical Reviewer

Dr. Lei Deng is an assistant professor within the Thoracic, Head & Neck medical oncology group at the University of Washington and Fred Hutchinson Cancer Center. He is interested in clinical and translational thoracic cancer research focusing on novel biomarkers and therapeutics, particularly KRAS-mutated and MTAP-altered lung cancer. He is also interested in optimizing systemic therapy for patients undergoing curative surgery and definitive radiotherapy. Dr. Deng co-leads the early-career working group at IASLC's Career Development Committee since 2025.