The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
Highlights of ASCO Gastrointestinal Cancer Symposium 2026: From Bench to Bedside
Assistant Professor of Medicine
Medical Oncologist
The 2026 ASCO Gastrointestinal Cancers Symposium showcased pivotal clinical trial data poised to reshape the treatment of gastric, colorectal, pancreatic, and liver cancers, highlighting advances in targeted therapy, immunotherapy, and biomarker-driven care.
The 2026 American Society of Clinical Oncology (ASCO) Gastrointestinal (GI) Cancers Symposium just concluded in San Francisco, CA. Themed "Meeting the Moment: Cancer Research Shaping the Future of Patient Care," the conference showcased the latest advancements in treating GI cancers, including pancreatic, liver, colorectal, and neuroendocrine tumors.
Here are some highlights from the presented clinical trial studies poised to transform practice.
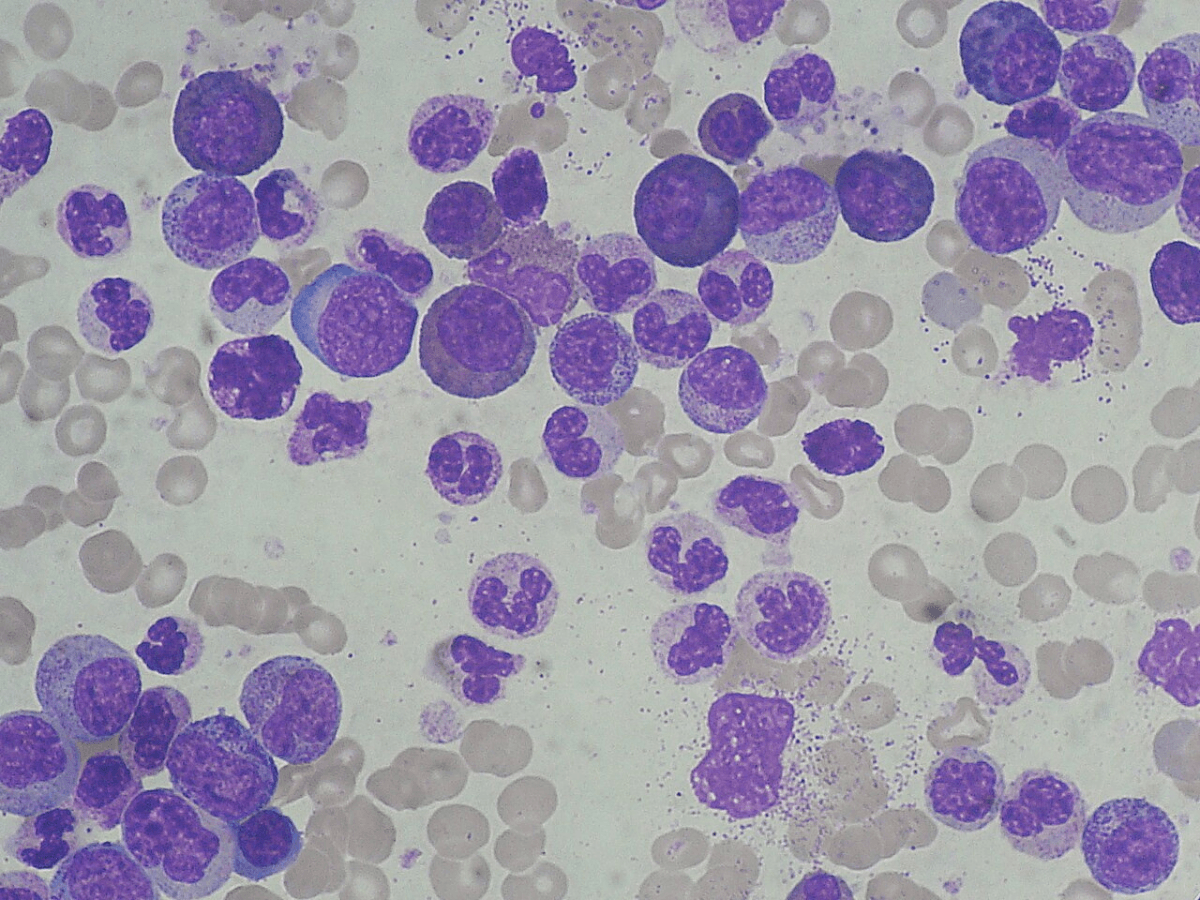
HERIZON GEA 01 TRIAL
This study was among the conference's highlights. This was a phase 3 study that investigated the efficacy of zanidatamab plus chemotherapy, with (triplet) or without (doublet) tislelizumab, compared with the SOC arm (trastuzumab plus chemotherapy) in treatment-naïve HER2+ metastatic GEA. Zanidatamab is a dual HER2 bispecific antibody that binds to extracellular domains 2 and 4 of HER2. Both zanidatamab-containing arms showed improved PFS (median PFS> 12 months) compared with trastuzumab, with a 35% reduction in the risk of progression or death. The triplet arm also showed a survival benefit compared to SOC, while the doublet arm showed a trend towards improved overall survival. As expected, the benefit was more pronounced in the HER2 IHC3+ group.
The caveat remains that the control arm lacked an immune checkpoint inhibitor in addition to chemo and trastuzumab, as is the current SOC for PD-L1-positive patients. It is reassuring that the PFS benefit was seen in the triplet arm despite the PD-L1 TAP scores. Exploratory analyses comparing the doublet and triplet arms would also provide further insight. While we still need to await the final analysis before changing the current SOC, this data could potentially change our current practice.
ILLUSTRO TRIAL
Results were presented for cohort 4 of this phase 2 study combining zolbetuximab with mFOLFOX6 and nivolumab in HER2-unresectable/metastatic gastric/GEJ adenocarcinoma with CLDN18.2 expression, and were compared with a historical control using chemo + zolbetuximab. The study met its endpoint with improved PFS (12.9 months). The benefit was more pronounced in patients with high CLDN 18.2 expression. It is noted that the current approval for zolbetuximab with chemo is for patients with high CLDN 18.2 expression. This combination adds another option for this population, particularly given that we do see about 20% of patients with multiple biomarkers positive. We need to await the data from the phase 3 trial with the same rationale comparing chemo with zolbetuximab to chemo with zolbe and pembrolizumab. It remains unclear whether the observed benefits are additive or synergistic, and further translational studies will likely provide more insight into the molecular underpinnings of treatment response noted with the anti-CLDN and anti-PD1 combination.
IKF-035/ABC-HCC TRIAL
This was a phase 3 study comparing TACE to systemic therapy with atezo/bev in intermediate-stage HCC. The median time to treatment failure was 14.6 months with atezo/bev compared to 9.5 months with TACE alone. There is a trend toward improved response, as systemic therapy is likely to address the multifocal nature of HCC. We will also need to take QOL into account, as the median number of cycles for atezo/bev was 12, compared to 2 for TACE. The generalizability of this data is also questionable, as more centers now favor radiation-based treatments such as Y90 or SBRT over TACE. The use of systemic therapy would also be limited based on baseline liver function; hence, patient selection would be key if considering incorporating this potential option in practice.
Phase 1 study of INCB161734[(KRAS) G12D inhibitor] in advanced/metastatic pancreatic duct adenocarcinoma
Interesting results were presented from this phase 1 study. In a heavily pretreated population, monotherapy with this novel agent showed a good response, with an ORR of 37% and a DCR of 78%, and a tolerable side-effect profile. The ongoing dose-escalation phase, using this agent in combination with chemotherapy regimens in first line and beyond, also showed encouraging responses, with no reduction in chemo due to toxicity. While the response rates seem promising, we do need to await more data from larger studies. It is truly exciting to have the potential to add various KRAS inhibitors, currently under investigation, to our list of treatments for this fatal disease.
COMMIT II
This was a phase 3 study evaluating the efficacy of FOLFOX with bevacizumab and atezolizumab, or atezolizumab alone, compared with FOLFOX/Bev alone in dMMR/MSI-H metastatic CRC. Due to a change in the standard of care following the Keynote 177 study, the FOLFOX/Bev arm was closed. The combination arm showed improved PFS compared to atezo monotherapy with a hazard ratio of 0.439. Interestingly, the atezo monotherapy arm underperformed significantly with a median PFS of 5.3 months. For context, the median PFS for Pembro in Keynote 177 was 16.5 months, whereas it was 39 months with nivolumab alone in CheckMate 8HW. This points to a potential limitation of PD-L1 blockers and raises questions about the use of other immune checkpoint inhibitors in the adjuvant setting for resectable dMMR/MSI-H colon cancers. Although the study demonstrated activity of platinum-based chemotherapy in patients with MSI-H CRC, at this time, it is unlikely to change practice, as other randomized controlled trials have shown the superiority of chemotherapy-free approaches over chemotherapy, with highly durable responses.
BREAKWATER
The primary analysis for cohort 3 from the BREAKWATER trial was presented, comparing FOLFIRI+EC to FOLFIRI+Bev in untreated BRAF V600E-mutant mCRC. Response rates improved with the addition of EC. There was a trend towards improved survival; however, the data are not yet mature. About a quarter of our patients receive FOLFIRI backbone at diagnosis; therefore, data supporting the addition of EC to this regimen are needed. The results of this study may be particularly important for patients with pre-existing neuropathy who are not eligible for oxaliplatin, and the FOLFIRI chemotherapy backbone may offer an alternative combination for EC if follow-up results validate the early findings presented at ASCO GI 2026.
About Authors

Meghana Singh, MD, is an Assistant Professor of Medicine at the West Virginia University School of Medicine and a medical oncologist with the WVU Cancer Institute, specializing in gastrointestinal malignancies. She received her medical degree from Osmania Medical College, completed her internal medicine residency at the University of Connecticut—where she also served as Chief Resident—and pursued fellowship training in hematology and oncology at the University of Pittsburgh Medical Center. During fellowship, she was selected to participate in the prestigious ASCO–AACR Clinical Trials Workshop and the ASCO SCION Workshop. Her academic interests include clinical trials, translational research, and improving access to high-quality cancer care across academic and community settings.
Ibrahim Halil Sahin, MD, is a medical oncologist specializing in gastrointestinal oncology. He is extensively involved in clinical trial development for colorectal cancer and nationally recognized expert in colorectal cancer. Dr. Sahin’s clinical and research interests focus on colorectal cancer, designing clinical trials with immunotherapy and targeted therapy for patients with advanced-stage colorectal cancer. He is an active member of the NCI Colon Task Force and Alliance Gastrointestinal Cancer and Colorectal Cancer Committees. He also currently serves as co-chair of the HCRN Gastrointestinal Clinical Trial Working Group. Board-certified in medical oncology and internal medicine, he received his medical degree from Hacettepe University School of Medicine in Ankara, Turkey.
Dr. Sahin completed two years of postdoctoral fellowship in the Gastrointestinal Oncology Department/Experimental Therapeutics Department at MD Anderson Cancer Center, and an internal medicine residency at the Icahn School of Medicine at Mount Sinai. He completed a hematology/oncology fellowship at Emory University School of Medicine, during which he received the ASCO Conquer Cancer Merit Award and the Rochfort scholarship. In addition, Dr. Sahin was selected to participate in the AACR/ASCO Methods in Clinical Research Workshop in 2019. His focus of research in colorectal cancer is precision medicine and immunotherapeutics, and he has been actively involved in drug development in this space.