The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
What Are Doctors Saying About Cancer Prevention? Insights from Leading Oncologists
Cancer prevention is not just about avoiding disease—it is about supporting patients throughout treatment and survivorship. At a major oncology conference, leading oncologists from NCI-designated cancer centers shared candid insights on exercise, alcohol use, treatment-related weight gain, and the critical gaps in survivorship care that continue to challenge patients and providers alike.
Experts from NCI-designated cancer centers discuss lifestyle interventions, treatment-related weight gain, and critical gaps in survivorship care
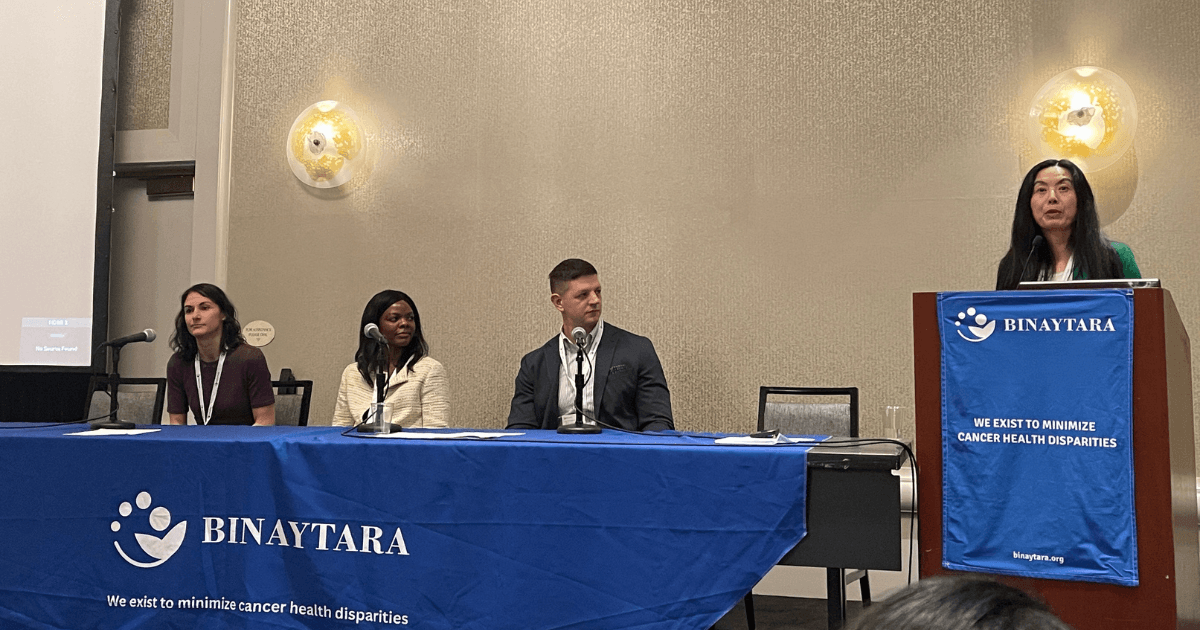
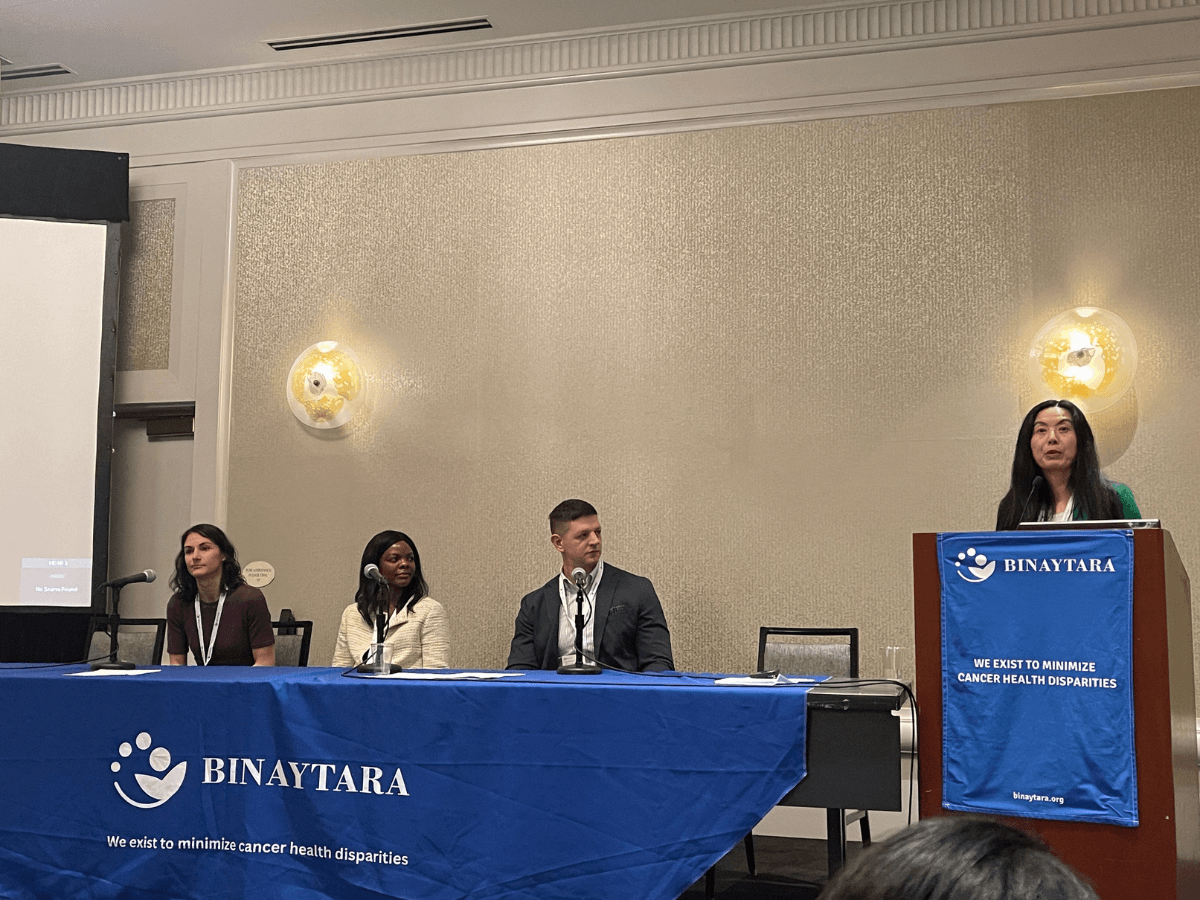
Pictured from left to right: Darien Reed-Perino, PhD, MD (Fred Hutchinson Cancer Center / University of Washington School of Medicine); Natasha Kwendakwema, MD (Fred Hutch / UW); Marko Velimirovic, MD (Fred Hutch); Fengting Yan, MD (Swedish Cancer Institute); discussing the importance of lifestyle factors in breast cancer care (update from San Antonio Breast Cancer Symposium 2025).
Oncologists from leading NCI-designated cancer centers engaged in a revealing discussion about cancer prevention and the real-world challenges patients face during treatment and survivorship. This discussion took place at the Best of Hematology & Breast Cancer 2026 conference in Seattle.
The conversation, which emerged during the breast cancer session, highlighted both evidence-based recommendations and honest acknowledgment of where the healthcare system falls short in supporting patients.
Does Exercise Prevent Cancer? Expert Consensus from Oncologists
When asked if they could only give one piece of advice to their patients about a lifestyle modification for cancer prevention, the experts reached immediate consensus: regular exercise.
Critically, they emphasized that physical activity's protective benefits extend beyond weight loss, a distinction that challenges common assumptions about why exercise matters for cancer prevention.
"Regular exercise, regardless of whether it leads to weight loss," one oncologist stressed, reflecting growing evidence that exercise provides independent metabolic and immune benefits like reducing stress that help reduce cancer risk and improve outcomes.
Alcohol and Cancer Risk: Should You Quit Drinking to Prevent Cancer?
The discussion became more complex when considering how to counsel a patient with a body mass index (BMI) of 28 who consumes two alcoholic drinks daily.
While the patient falls into the overweight category, the panel leaned toward prioritizing alcohol reduction over weight loss, given emerging data on alcohol's direct carcinogenic effects. However, they acknowledged the ideal scenario would address both factors.
This exchange underscored a reality of clinical practice: cancer prevention and management require individualized approaches rather than one-size-fits-all recommendations.
Does Breast Cancer Treatment Cause Weight Gain? What Experts Say
An audience member raised what many breast cancer survivors know all too well: significant weight gain during hormonal therapy, which can occur within six months to two years of starting treatment.
The question struck at a fundamental tension in cancer care. Patients complete intensive treatment, only to struggle with side effects from the very medications designed to prevent recurrence, side effects that have gained increasing visibility through social media discussions.
One oncologist's response was notably candid about the gap in supportive care during this critical phase.
Life After Chemotherapy: What Oncologists Wish They Could Offer Patients
"When we are doing chemotherapy and intense treatments, we have really great support systems," the expert explained. "We manage symptoms, and patients are talking to our team constantly. Then they come out of that, and we give them medical therapy that makes them feel not great and causes weight gain."
The standard recommendations—exercise, reduce alcohol consumption, see a nutritionist—often fall short, not because patients lack knowledge, but because the support infrastructure does not match the challenge.
"With some exceptions, most people know healthy choices to some degree. That's not the problem," the oncologist continued. "I think we can go a long way in having better support systems for our patients in that stage of disease."
Ozempic for Cancer Patients: Can GLP-1 Drugs Help Treatment-Related Weight Gain?
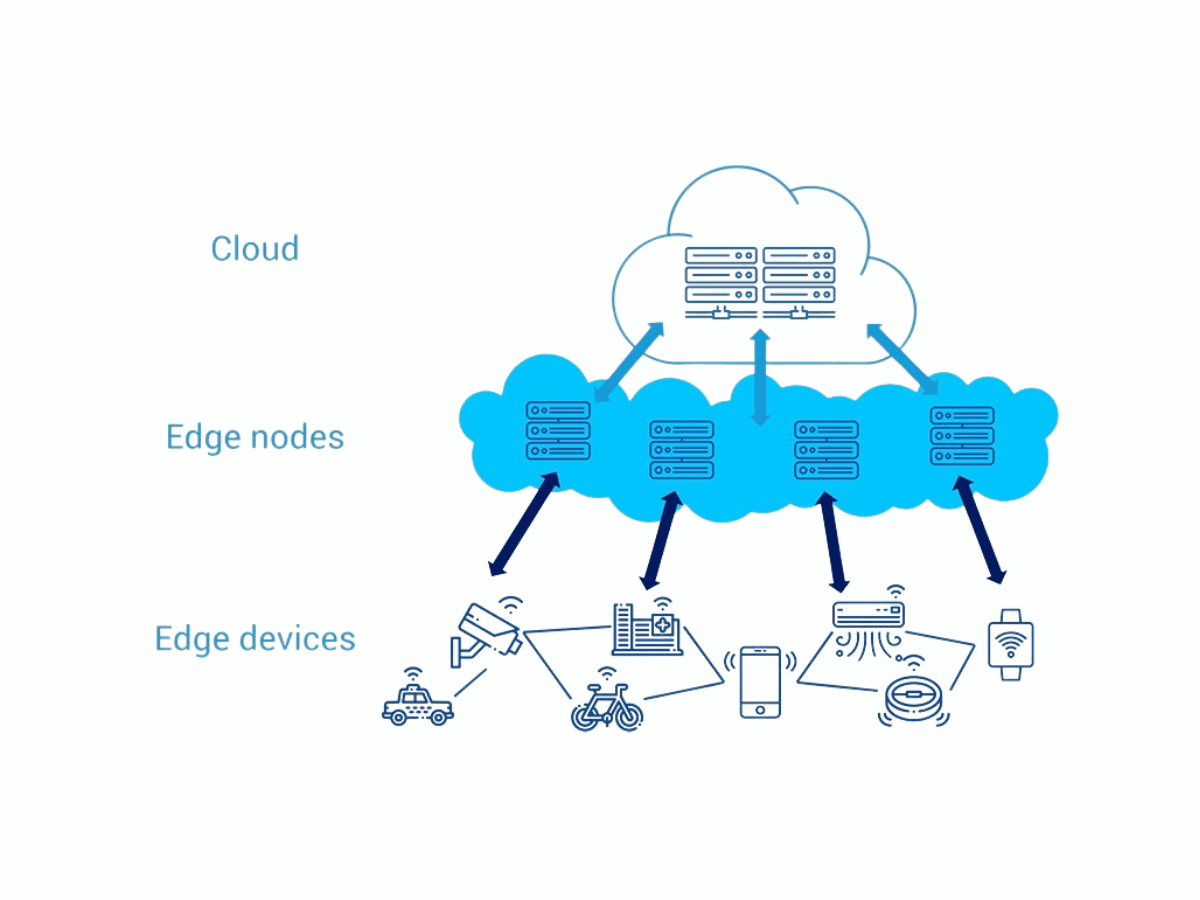
The panel pointed to potential advances, including GLP-1 receptor agonists (medications like semaglutide and tirzepatide) currently being studied in cancer populations, as well as improved access to comprehensive survivorship programs.
However, they acknowledged a fundamental barrier: adherence becomes nearly impossible when patients experience treatment-related joint pain, fatigue, and other side effects that make exercise feel insurmountable.
"They don't feel like exercising when their joints hurt and they are tired," one panelist noted. "So I struggle with that."
This honest acknowledgment from experienced oncologists reveals that the challenge of survivorship support is systemic, not individual.
What This Means for Patients and Providers
The discussion at this major oncology conference illuminates several critical points:
For Prevention: Regular physical activity remains the most evidence-based lifestyle intervention, with benefits independent of weight loss. Alcohol reduction should be prioritized given its direct links to multiple cancer types.
For Survivors: Weight gain during hormonal therapy is a recognized medical issue, not a failure of willpower. The current gap between intensive treatment support and survivorship care needs to be addressed at a healthcare system level.
For the Field: Oncologists at leading institutions are actively seeking better tools—whether novel medications, enhanced support programs, or multidisciplinary approaches—to help patients navigate the challenging transition from active treatment to long-term survivorship.
The Future of Cancer Prevention: Better Support Systems for Lifestyle Changes
While the evidence supporting lifestyle interventions for cancer prevention continues to strengthen, the healthcare system must develop more robust, practical support mechanisms for patients attempting to implement these changes, particularly those managing treatment-related side effects that make standard recommendations difficult to follow.