The Cancer News
AN AUTHORITATIVE RESOURCE FOR EVERYTHING ABOUT CANCER
Dr. Matthew H. Schwede’s Insights on Advances in Cellular Therapy
Cellular therapy is entering a new era marked by faster manufacturing, safer products, and earlier use in treatment. In this conference summary from the Best of Hematology & Breast Cancer 2026 meeting, Dr. Matthew H. Schwede highlights key advances in CAR T-cell therapy, including rapid turnaround products, in vivo CAR T, dual targeting strategies, and expanding applications beyond traditional B-cell malignancies—developments that are poised to reshape clinical practice over the next several years.
This article summarizes the presentation by Dr. Matthew Harold Schwede (Swedish) at the Best of Hematology & Breast Cancer 2026, Seattle conference. It has not been reviewed by the speaker and may contain errors.
The field of cellular therapy continues to evolve rapidly, with numerous updates presenting exciting new concepts and approaches. Rather than examining every individual study in detail, this overview focuses on the major ideas shaping the field and the research supporting these developments.
Optimizing Current CAR T-Cell Products Through Earlier Administration
One of the most significant findings involves improving outcomes with existing products by administering them earlier in the treatment timeline. Research examining cilta-cel in multiple myeloma compared results from two trials where the therapy was given at different stages. In one trial, cilta-cel was administered in later lines of therapy (three or four or more lines), while in another study, it was given earlier.
The results demonstrated that patients generally experienced better outcomes when cilta-cel was administered earlier. More patients achieved longer survival when the therapy was given after one prior line of therapy compared to two, three, or four prior lines. While this finding may not be entirely surprising—therapies across all cancers are often more effective in earlier lines—the research provided compelling correlative evidence using RNA sequencing and other translational tools.
The analysis revealed better immune cell fitness of peripheral T cells when treatment was given earlier, including more CD4-positive naïve T cells and improved tumor microenvironment characteristics, specifically more tumor-associated macrophages. These findings suggest that earlier administration is more effective, potentially due to these immune and tumor microenvironment changes.
Combination Strategies: CAR T Followed by Bispecific Antibodies
Another approach to maximizing the effectiveness of existing products involves sequential therapy combinations. One study examined administering a BCMA CAR T followed by a bispecific antibody. The bispecific antibody was given approximately two and a half months after the CAR T infusion. In this case, the bispecific antibody cevostamab targets FFCRH5, a receptor expressed on myeloma cells that is independent of BCMA and widely expressed.
This single-arm study demonstrated a very high early negativity rate at one year, and the approach was generally well tolerated. However, there were some unusual immune adverse events, including neuropathy with ataxia, autoimmune hepatitis, and colitis—conditions rarely seen with CAR T cells alone. While these events were reversible, they represent an important consideration. This concept of CAR T followed immediately by bispecific therapy is being explored across multiple types of hematologic malignancies.
Rapid Manufacturing: Fast CAR T Products
The development of very quick turnaround products represents a significant advancement, eliminating the need for bridging therapy during the manufacturing wait period. One notable example is Fast CAR T, a product for multiple myeloma targeting both BCMA and CD19. This product also incorporates the concept of dual targeting and early administration.
In this approach, patients with newly diagnosed multiple myeloma received two cycles of lenalidomide, bortezomib, and dexamethasone—a standard therapy regimen. This could be administered before or after apheresis. Patients then received standard lymphodepletion with fludarabine and cyclophosphamide, followed by the CAR T infusion. Lenalidomide maintenance was permitted for up to two years per investigator's discretion. The remarkable aspect of this product is that manufacturing was completed in less than three days, with a median time from diagnosis to infusion of approximately three months.
The safety profile was favorable, with only about one-third of patients experiencing cytokine release syndrome (CRS), all of which was low grade. No immune effector cell-associated neurotoxicity syndrome (ICANS) occurred, despite targeting two different receptors. Unlike some other BCMA CAR products, no delayed neurotoxicity was observed, and no secondary primary malignancies were reported, though follow-up remains limited.
Adverse events were primarily cytopenias, with most other toxicities being low grade except for infections. The efficacy results showed very high overall response rates and high MRD negativity in newly diagnosed patients, with negativity generally sustained at one year.
The Rationale Behind Rapid Manufacturing
Beyond the convenience of faster product availability and avoiding the five-week wait and bridging therapy considerations, there is scientific evidence supporting rapid manufacturing. The hypothesis suggests that manufacturing CAR T cells more rapidly preserves more naïve T cells—youthful T cells that may be more potent and active.
Studies of rapidly manufactured CD19-targeting products in various liquid malignancies and diffuse large B-cell lymphoma have demonstrated high response rates without significant toxicity. One particularly impressive aspect is the speed: median time from leukapheresis to delivery was nine days, effectively eliminating the need for bridging therapy. Multiple studies are currently exploring this rapid manufacturing approach.
In Vivo CAR T: A Paradigm Shift
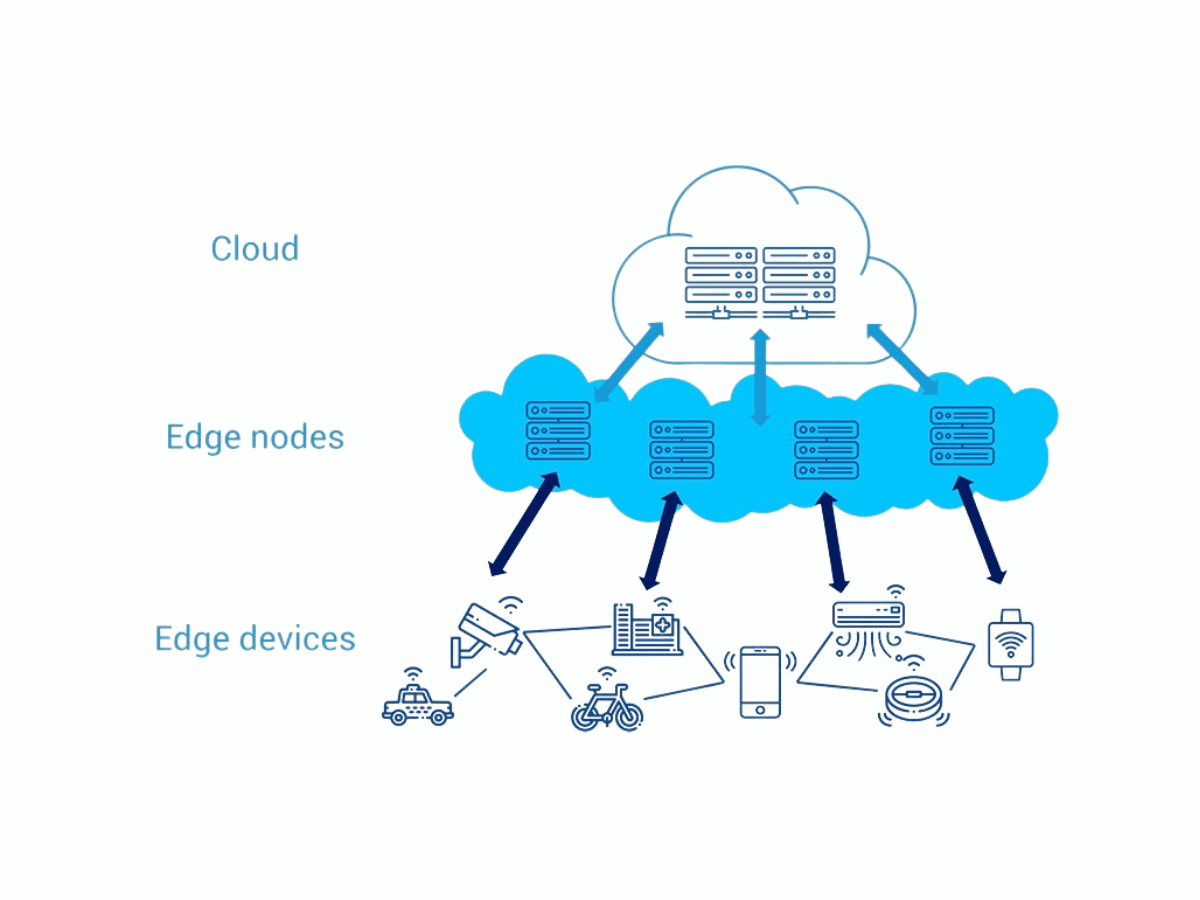
One of the most exciting early-stage developments is in vivo CAR T therapy. A phase one study with four patients examined this approach in relapsed/refractory multiple myeloma. Instead of manufacturing CAR T cells ex vivo and infusing them weeks later, this approach involves administering a lentivirus that enables the patient's own T cells to express a CAR receptor in their body.
The lentivirus carries a BCMA CAR with a 4-1BB costimulatory domain and includes a receptor targeting CD3 to specifically transduce T cells. The design modifies the lentivirus to avoid the LDL receptor it normally targets, directing it instead to T cell receptors. This approach potentially eliminates the need for lymphodepletion, potentially reducing costs and manufacturing complexity.
Patients with relapsed/refractory multiple myeloma who had received at least three prior lines of therapy were enrolled. All four patients achieved MRD negativity at one month—a highly encouraging result. Remarkably, toxicity was minimal, with no ICANS and only low-grade CRS in all four patients. Unlike lymphodepleting chemotherapy followed by CAR T, there were minimal cytopenias. Grade three or higher cytopenias were extremely rare, countable on one hand across the four patients.
The study demonstrated significant lymphocyte expansion following the in vivo CAR infusion, with one patient's lymphocyte count reaching approximately 45,000. While there were no clinical consequences of this lymphocytosis, some patients received dexamethasone to reduce the count. Analysis showed substantial expansion of lymphocytes after infusion, with CD3-positive cells in some patients being predominantly CAR-positive, and a substantial minority being CAR-positive in other patients.
By targeting CD3, the approach creates both CD8-positive and CD4-positive T cells expressing the CAR, resulting in a mixed population of CAR-expressing T cells.
Dual Targeting: Multiple Antigens or Sequential Infusions
An increasingly popular approach involves targeting two antigens either with a single dual-targeting CAR or through sequential infusions of different CAR products. One study examined sequential CAR infusions in multiple myeloma patients with at least three prior lines of therapy and very bulky extramedullary disease—generally a poor prognosis population.
The strategy involved giving two different CAR products: one targeting BCMA and another targeting GPRC5D on days zero and one, respectively. The treatment protocol first included debulking chemotherapy (DCP) followed by radiation to the dominant extramedullary lesion, both to reduce tumor burden and potentially create a more favorable tumor microenvironment. Standard lymphodepletion chemotherapy preceded the CAR infusions, with the primary endpoint being overall response rates.
While the sample size was small and single-arm (not compared to a control), most patients achieved a complete metabolic response despite their typically poor prognosis. There were infections and grade three hematologic toxicities as expected, but responses generally lasted several months, suggesting promise for this approach in overcoming antigen loss, such as BCMA loss at relapse.
Single Products with Dual Targeting
Rather than sequential infusions, several combined CD19/CD20 CAR T-cell products are in development. One example includes two variants: KITE-363 and KITE-753, with the latter being a rapidly manufactured product. The phase one dose escalation study used approximately tenfold lower doses for the rapidly manufactured variant, based on the hypothesis that rapid manufacturing preserves more naïve, youthful, active T cells.
Both products incorporate different costimulatory domains: CD28 for CD19 and 4-1BB for CD20. Despite the significantly lower dose of KITE-753, robust expansion was observed at all dose levels, occurring despite the ten-fold dose reduction. Response rates were generally high among CAR-naïve patients in this dose escalation study, though previously CAR-exposed patients had limited responses. Consistent with other recent studies, toxicity was not extensive.
Alternative Targets: BAFF Receptor CAR T
CD19-negative relapse represents a significant problem in lymphoma treatment. BAFF receptor (BAFFR) is often still present on lymphoma cells even when CD19 is lost. Unlike CD19, which is not essential for B-cell function, BAFFR is essential, making it an attractive alternative target.
A small study of nine patients, mostly with mantle cell lymphoma, included four who had received prior CD19 CAR therapy. Interestingly, high BAFFR expression was not required; patients with relatively low BAFFR expression still appeared to benefit in this limited sample. Toxicity was quite low, suggesting that outpatient CAR T administration could be feasible. Though the study was a phase one dose escalation with a small sample size, the complete response rate was approximately 100% so far, including in some CAR-exposed patients.
IL-18 Armored CAR T Cells
IL-18 armored CAR T cells represent an innovative approach where CAR T cells also express IL-18. Through multiple mechanisms, IL-18 augments the anti-tumor effect of CAR T cells and potentially leads to longer persistence. Several studies have explored IL-18 armored CARs in various lymphoid diseases.
Published research has demonstrated that CD19 CARs with IL-18 could effectively treat patients who had previously been exposed to CD19 CAR therapy. Additional studies in chronic lymphocytic leukemia (CLL) showed promising results. While the overall response rate of 43% in patients exposed to BTK inhibitor and venetoclax may not seem remarkable, it represents a significant improvement over standard CAR T cells, which are typically only about 20% effective in CLL. This product also features an expedited three-day manufacturing process. Notably, there was no increase in systemic IL-6 elevation, hemophagocytic lymphohistiocytosis, or other significant toxicity, with adverse events being manageable.
Expansion Beyond B-Cell Malignancies: CD7 CAR T in AML and T-ALL
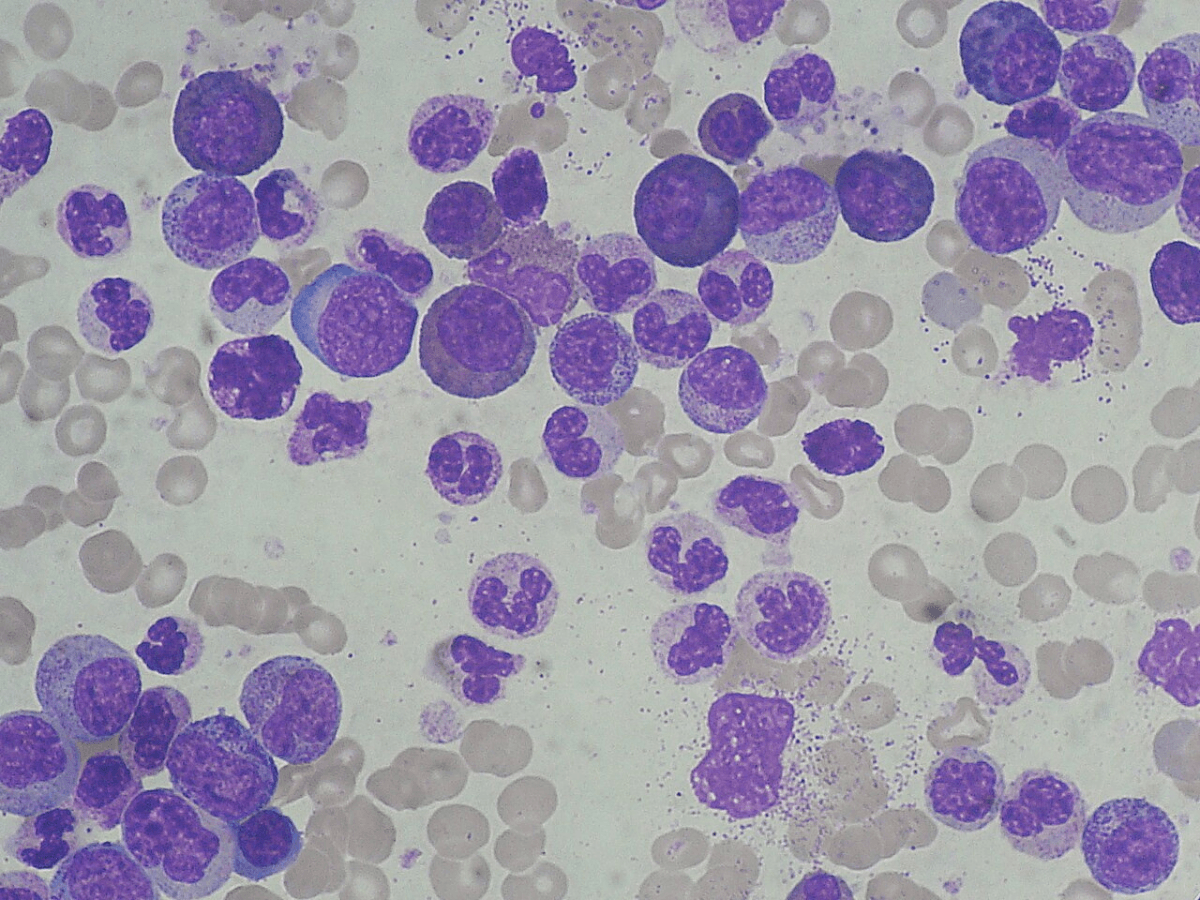
CAR T-cell therapy is expanding beyond myeloma and B-lymphoid malignancies. Multiple studies have examined CD7 CAR T cells. CD7 is expressed on T cells and NK cells, and on approximately one-third or more of acute myeloid leukemia (AML) cells. It is also universally expressed on T-cell acute lymphoblastic leukemia (T-ALL) cells.
To make this approach viable, T cells must be edited to eliminate CD7 expression and the T-cell receptor. This editing enables eventual allogeneic off-the-shelf production. By removing the T-cell receptor to prevent graft-versus-host disease and editing out CD7 so the CARs do not attack themselves, donor-derived CAR T cells can be created for T-ALL and some AML cases.
Multiple ongoing phase one studies are exploring CD7 CARs. Results have been promising, with at least half, and likely most, patients achieving complete responses or significant benefits. Toxicity profiles have been generally favorable, though viral reactivation is common—not surprising given that CD7 is being targeted on immune cells. This approach offers a potential bridge to allogeneic transplant for many patients and represents an exciting possibility for T-ALL and AML, diseases that currently lack effective CAR T-cell options.
Consolidative CAR T in ALL
An emerging application involves using CAR T cells for consolidation in patients who have achieved MRD negativity after induction or early treatments. Multiple abstracts presented data on acute lymphoblastic leukemia (ALL) patients who, after achieving MRD negativity, received CAR T for consolidation rather than undergoing numerous consolidation cycles and years of maintenance therapy.
These small, single-arm studies have shown very high progression-free survival rates at one year. This represents a potentially transformative use of CAR T cells—consolidating remission in the MRD-negative setting to avoid years of subsequent therapy that ALL patients typically receive. This approach will likely expand to other diseases beyond ALL in the coming years.
Implications for Clinical Practice
These developments carry several important implications for clinical practice. First, there is growing evidence for administering CAR T therapies earlier in the treatment course. Clinicians should consider how to facilitate patient access to centers offering CAR T or enroll them in trials investigating earlier CAR T administration, as this approach shows considerable promise.
Many of these CAR T products demonstrate favorable safety profiles, making them viable options for elderly patients or those who may not tolerate very intensive therapy. The field is experiencing rapid innovation across multiple fronts: dual targeting approaches, faster turnaround times, safer products, more effective utilization strategies, and earlier administration.
Looking ahead to the next three to five years, the landscape will likely shift dramatically. The five-week wait for CAR T cells and the need for bridging therapy considerations will probably diminish as rapid turnaround products replace current manufacturing timelines. While the field continues to refine optimal utilization of these products given the numerous emerging approaches, the trajectory is clearly toward faster, safer, and more effective cellular therapies that can be deployed earlier in the disease course and across an expanding range of hematologic malignancies.